Page Contents
OVERVIEW
Before any procedure it is important to make sure to look through relevant prior imaging to be thorough. While a paracentesis is a simple procedure, this concept still applies here. This page will review some of what can be reviewed on imaging prior to performing a paracentesis. For further reference, the page on the radiological appearance of ascites can be referenced. This page focuses on aspects of reviewing imaging that are most relevant for the paracentesis procedure, for a more general overview of how to review prior imaging imaging for radiology procedures please refer to this page: Fundamental Procedural Radiology Peri-Procedural Tasks: Reviewing Relevant Prior Imaging.
It is also very important to realize that reviewing prior imaging is a core component of performing a pre-procedure chart review in a patient for a paracentesis, which is covered in more detail on its separate linked page.
INITIAL QUESTION: HAS THE PATIENT EVEER HAD A PARACENTESIS BEFORE?
In many cases patients who are going to receive a paracentesis have had one previously. It is very helpful to look back and see if the patient has ever received a paracentesis in the past as it can save considerable time and can help answer some key questions such as:
- How long ago was their last paracentesis (how often do they get a paracentesis, and is it on a regular interval)? This can give a sense of timing of paracentesis and the interval they require for the drainage of their ascites.
- How much volume was removed during their last paracentesis? Combined with how long ago this was done, knowing the volume drained previously can help inform how much you may expect during their current procedure.
- What did the ascites look like? This is often charted with the volume removed. This can also set expectations on what you might see when draining their ascites for the current procedure.
- Was albumin given and if so, how much? While there are guidelines for the administration of albumin in the setting of paracentesis it is always useful to contextualize what patients have received previously (and how it was tolerated).
ESSENTIAL QUESTION: DOES THE PATIENT EVEN HAVE ASCITES (OR ENOUGH ASCITES TO DRAIN)?
Perhaps the most pertinent question that can be answered by reviewing imaging prior to a paracentesis is to establish if the patient even has ascites to begin with. It may seem obvious that this should be checked, however sometimes patients may have a physical exam that suggests ascites, but on imaging there may not be ascites present. And sometimes, even if there is ascites, the volume may not be large enough to safely perform a paracentesis.
Whenever possible, it can be useful to establish this information with prior diagnostic imaging (instead of bringing down the patient for the procedure, and discovering last minute that there is not any ascites/enough ascites to drain easily.
Ascites is commonly detected by ultrasound or by CT scan, this is covered more below.
EVALUATING ASCITES ON ULTRASOUND:
Prior ultrasound studies may have demonstrated that their was ascites present. It is important to realize that that ascites should should appear anechoic on ultrasound as it is a simple fluid.
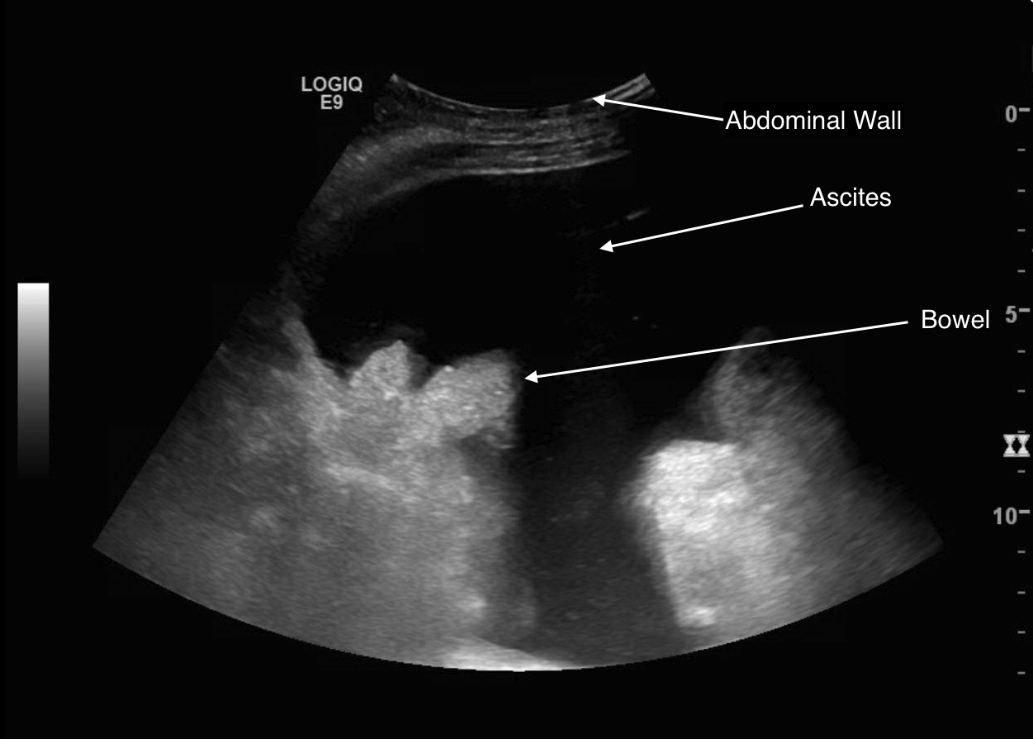
The relative amount and location of ascites can be demonstrated on a prior ultrasound study, however it is important to realize that ascites can move around, and change location with patient positioning.
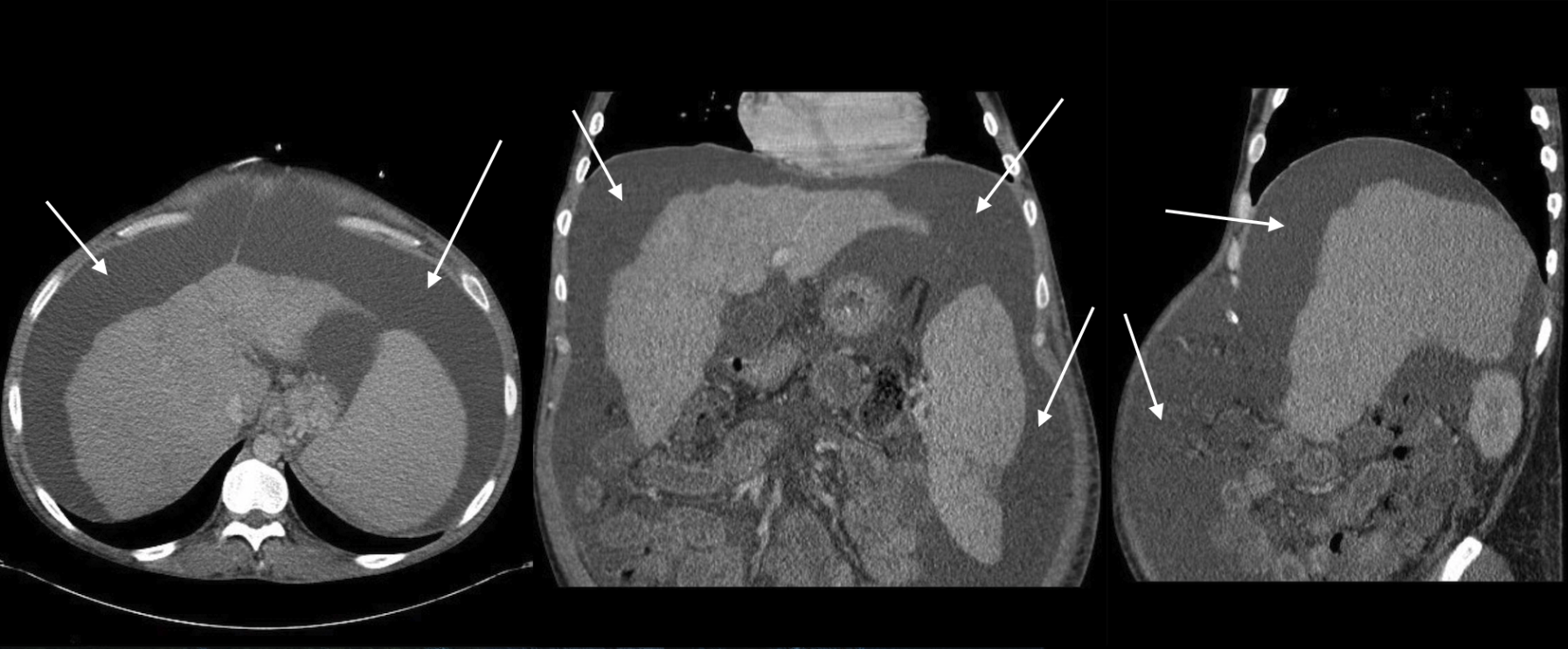
EVALUATING ASCITES ON CT SCAN:
Sometimes ascites will be seen on CT scan studies. It is pertinent to keep in mind that the density of ascites (Hounsfield units/HUs) should be similar to that of water (-10 to 10 HU). In cases of more exudative ascites, the density can be higher (going to 15 HU as above) as the amount of protein in the ascites is more.
OTHER ANATOMICAL CONSIDERATIONS:
Prior imaging may also reveal other anatomical considerations that can be useful to keep in mind when planning the prospective approach to draining the ascites fluid. These can include:
- Depth of the ascites: how deep must the needle travel before reaching the pocket of ascites safely?
- Large superficial collateral vessels: it can be useful to make sure to avoid any large superficial collateral vessels that may have developed in the setting of portal hypertension (and will bleed if punctured by a paracentesis needle).
Page Updated: 09.01.2019