Page Contents
- 1 WHAT IS IT?
- 2 WHAT CAUSES IT?
- 3 WHY IS IT A PROBLEM?
- 4 WHAT MAKES US SUSPECT IT?
- 5 CLINICAL WORKUP
- 6 AT WHAT POINT DO WE CONFIDENT IN MAKING THE DIAGNOSIS?
- 7 WHAT ELSE ARE WE WORRIED ABOUT?
- 8 HOW DO WE TREAT IT?
- 9 HOW WELL DO THE PATIENTS DO?
- 10 WAS THERE A WAY TO PREVENT IT?
- 11 ARCHIVE OF STANDARDIZED EXAM QUESTIONS
- 12 FURTHER READING
WHAT IS IT?
A simple partial seizure is a type of focal seizure that can occur in patients. It is fundamentally characterized by the fact that it does NOT cause a lose in consciousness.
WHAT CAUSES IT?
This type of seizure (given that it is focal) is caused by abnormal activity in a single area of the brain. The exact focal region of the brain involved can be variable.
What causes the abnormal activity? This question is a valid one, and will require investigation to figure out. Seizures can be causes by systemic processes (such as electrolyte disturbances) or even masses within the brain. The EXACT cause is not always clear!
WHY IS IT A PROBLEM?
These types of seizures can be disruptive. What’s more, simple partial seizures can secondarily generalize and begin to involve the whole brain/body.
WHAT MAKES US SUSPECT IT?
Common Chief Complaints:
- Episodes of muscle jerking
- Suspected seizures
History Of Present Illness
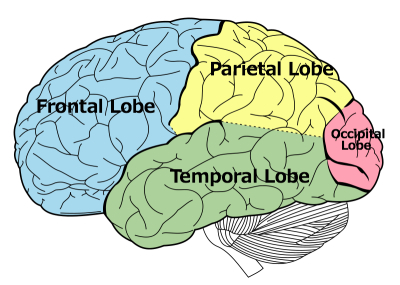
Nature of seizure: the symptoms experienced by patients can include motor, sensory, autonomic, or psychological symptoms (these will vary depending upon the location of the seizure activity in the brain).
- Motor: isolated regions of muscle jerking that can spread (Jacksonian march)
- Sensory: tingling can be present in regions such as the hand
- Autonomic (insular cortex involvement): changes in blood pressure, changes in heart rate, bronchoconstriction.
- Psychological: fear, déjà vu, hallucinations
No loss of consciousness: patients who have simple partial seizures will remain conscious during the seizure (even when hallucinating).

Postictal focal neurological deficit: patients can experience these types of deficits immediately after the seizure (that usually remove in 24 hours). These are often confused for symptoms of a stroke.
- Todd’s paralysis: often characterized by a focal weakness that affects an appendage unilaterally.
- Hemiplegia/hemiparesis: depending on the nature of the seizure their may be a more widespread paralysis
Physical Exam Findings
Physical exam findings will depend on the underlying cause of the seizure.
CLINICAL WORKUP
The initial goal of workup will be to try and rule out systemic causes for the seizure:
Fingerstick glucose: patients with abnormal blood sugars may present with seizures, and this study can easily evaluate for hypoglycemia/hyperglycemia.
Basic metabolic panel (BMP): ordering this study will help to asses for electrolyte imbalances that can be responsible for inducing seizures.
Liver function tests (LFTs): hepatic encephalopathy can sometimes be responsible for precipitating seizures.
Toxicology screen (urine/serum): evaluating for the presence of various compounds in patient serum/urine can help evaluate for seizure activity that is related to ingestion of toxins/medications.
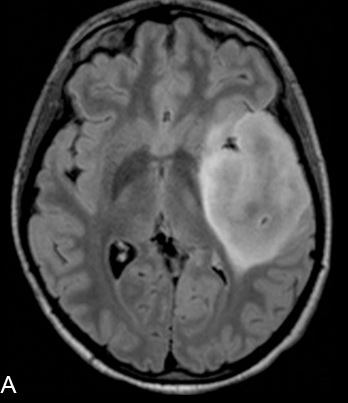
Another important goal will be to rule out a mass in a focal region of the brain:
MRI imaging can be use to evaluate for the presence of any pathology that might explain the seizure activity.
Along with the goals above, we must also confirm seizure activity:
EEG: ordering this study will often be able to confirm a focal location of abnormal brain activity.
AT WHAT POINT DO WE CONFIDENT IN MAKING THE DIAGNOSIS?
With a clear history (no loss in consciousness of course), and EEG findings that support focal seizure activity, the diagnosis can be made.
WHAT ELSE ARE WE WORRIED ABOUT?
Generalization of focal seizures: patients with a focal seizure can have it generalize.
Patients driving: in some states (such as Massachusetts) patients must refrain from deriving for 6 months after having a seizure (and must be seizure free in that time period before returning to the roads).

HOW DO WE TREAT IT?
For children:
Phenobarbital is typically the first-line anticonvulsant that is used in children.
General medical treatment options:
Carbamazepine is a anticonvulsant that is used specifically for focal seizures.
Phenytoin: this medication is another treatment option. It does not have to be titrated and can be given at its therapeutic dose quickly.
Seizures refractory to medication:
Lobectomy: in cases where the seizure activity is not well controlled with medications.
HOW WELL DO THE PATIENTS DO?
Prognosis is variable and depends upon the clinical context.
WAS THERE A WAY TO PREVENT IT?
Some systemic causes of seizures (electrolyte imbalances, drug overdose) are avoidable.
ARCHIVE OF STANDARDIZED EXAM QUESTIONS
This archive compiles standardized exam questions that relate to this topic.
FURTHER READING
Page Updated: 08.06.2016