Page Contents
- 1 WHAT IS IT?
- 2 WHY IS IT A PROBLEM?
- 3 WHAT MAKES US SUSPECT IT?
- 4 CLINICAL WORKUP
- 5 AT WHAT POINT DO WE CONFIDENT IN MAKING A DIAGNOSIS?
- 6 WHAT ELSE ARE WE WORRIED ABOUT?
- 7 HOW DO WE TREAT IT?
- 8 HOW WELL DO THE PATIENTS DO?
- 9 WAS THERE A WAY TO PREVENT IT?
- 10 OTHER HY FACTS?
- 11 ARCHIVE OF STANDARDIZED EXAM QUESTIONS
- 12 FURTHER READING
WHAT IS IT?
Alzheimer disease (AD) is a degenerative disease of the cortex that is the most common cause of dementia. It is believed that this condition can be caused by the deposition of amyloid-β protein (cleaved from amyloid precursor protein/APP) into brain tissues.
Neurotransmitter changes are observed in this condition:
- Acetylcholine is decreased (due to loss of cholinergic neurons ins the nucleus basalis of Meynert)
- Glutamate is increased
WHY IS IT A PROBLEM?
The amyloid proteins deposited into the brain in Alzheimer disease are believed to be neurotoxic and cause a host of neurological problems (explained more below).
WHAT MAKES US SUSPECT IT?
Risk factors:
Down syndrome, elderly age, female sex, family history, ApoE4, APP, presenilin-1, presenilin-2
Protective factors:
ApoE2
Chief Complaints:
- Memory loss
- Language dysfunction
- Loss of motor skills
- Personality change
History Of Present Illness:
Disease onset is insidious and gradually progressive:
- Memory loss (typically anterograde not retrograde): this typically begins with short term memory loss, and progresses to longer term memory loss/disorientation (patients will forget where they are/get lost).
- Language dysfunction: as time goes on patients can even become mute
- Loss of motor skills: this can progress to the point that the patient may even become bedridden.
- Behavior/personality changes that can include agitation, psychosis, depression, paranoia, delusions, and sleep disturbances.
Physical Exam:
Mental status exam scores are often lowered.
Other physical exam components will generally be normal in these patients
CLINICAL WORKUP
Basic labs should be checked to rule out common issues:
- Serum TSH levels should be normal in patients with AD
- Vitamin B12 levels should also be normal
Neuropsychological testing can be useful in distinguishing demential from depression.
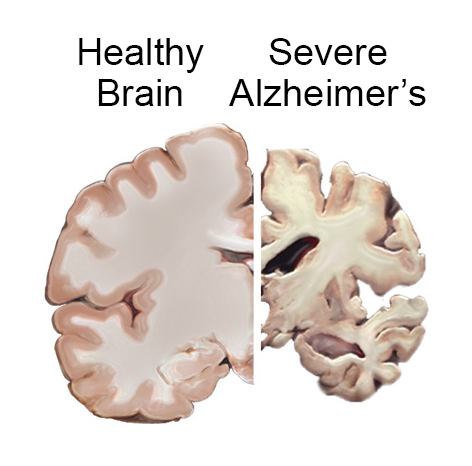
MRI imaging can reveal the presence of senile plaques (amyloid deposition) in the grey matter of the brain. General cerebral atrophy can also be observed (especially in the hippocampus).
PET imaging shows nonspecific bilateral temporoparietal hypo metabolism. This imaging modality is not necessary for everyone being worked up for AD, however if the study is collected, this is what can be observed.
AT WHAT POINT DO WE CONFIDENT IN MAKING A DIAGNOSIS?
AD is typically made based upon a clinical diagnosis: with a presentation consistent with AD (and in the absence of other reasons for dementia) patients will often be given the diagnosis of AD.
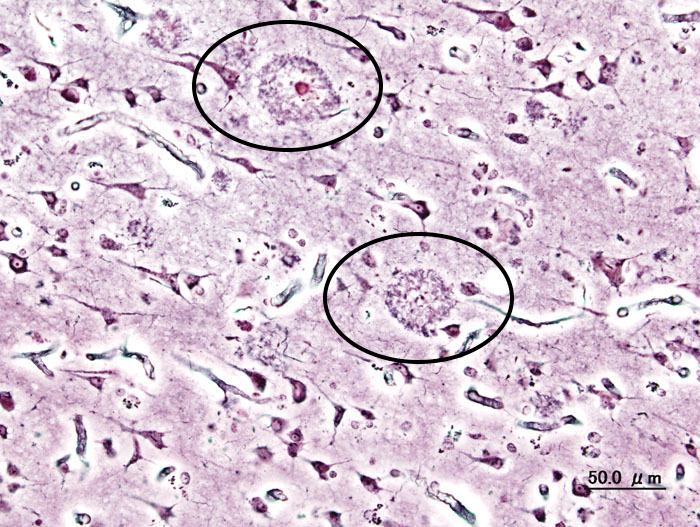
Histological findings (confirmatory at autopsy) include widespread cortical atrophy, narrowing of the gyri, and widening of the sulci. Other findings include:
- Amyloid-β depositions that are extracellular
- Neurofibrillary tangles which are intracellular hyperphosphorylated aggregates of tau protein (which essentially manifest as insoluble cytoskeletal elements). Generally, the more tangles the more advanced the degree of the dementia.
WHAT ELSE ARE WE WORRIED ABOUT?
Amyloid angiopathy may be caused due to the deposition of amyloid into the walls of cranial vessels. This can lead to intracranial hemorrhage
Infection is a common complication in patients who become bedridden (and lose significant language skills). Aspiration pneumonia is a common cause of death.
Usage of anticholinergic agents: patients with Alzheimer disease are usually sensitive to the deleterious effects of anticholinergic medications.
HOW DO WE TREAT IT?
Anticholinesterases (donepezil, galantamine, rivastigmine, tacrine) is used to increase acetylcholine signaling and are a common treatment modality for Alzheimer
Memantine is a NMDA receptor antagonist that helps prevent excitotoxicity. It is sometimes used for Alzheimer.
HOW WELL DO THE PATIENTS DO?
Alzheimer dementia is unfortunately an irreversible condition. Typically survival is int he range of 5-10 years form the onset of symptoms.
WAS THERE A WAY TO PREVENT IT?
*No clear way to prevent the onset of this condition.
Vitamin E (α-tocopherol) may slow cognitive decline.
OTHER HY FACTS?
Ex vacuo ventriculomegaly refers to the increased appearance of CSF on imaging that is seen when there is decreased brain tissue (such as in Alzheimer disease secondary to neuronal atrophy).
Early onset risk factors: APP, presenilin-1, presenilin-2
The gene for APP is present on chromosome 21. This is thought to explain the association with trisomy 21
Microglia cells are the resident macrophages of the brain and seem to be implicated in Alzheimer disease.
The locus ceruleus loses neurons in Alzheimer’s disease
ARCHIVE OF STANDARDIZED EXAM QUESTIONS
This archive compiles standardized exam questions that relate to this topic.
FURTHER READING
Page Updated: 06.29.2016