Page Contents
- 1 OVERVIEW
- 2 BASIC COMPONENTS
- 3 CHEST/PRE-CORDIAL LEADS
- 4 LIMB LEADS
- 5 HEART RATE
- 6 SINUS RHYTHM
- 7 AXIS OF HEART’S ELECTRICAL ACTIVITY
- 8 INTERVALS
- 9 MORPHOLOGY
- 10 ST SEGMENT ELEVATION
- 11 ST SEGMENT DEPRESSION
- 12 T WAVES
- 13 ATRIAL/VENTRICULAR BLOCK (AV BLOCK)
- 14 BUNDLE BRANCH BLOCKS (BBB)
- 15 POTASSIUM ABNORMALITIES
- 16 ATRIAL FIBRILLATION
- 17 ATRIAL FLUTTER
OVERVIEW
This page is dedicated to covering (in a comprehensive manner) all the topics that are relevant to reading an electrocardiogram. Look to this linked page for a more succinct guide on how to read an EKG quickly.
BASIC COMPONENTS
An electrocardiogram (EKG or ECG for short depending on where you are from) in a nutshell is a electrical snapshot/image of the hearts activity from a particular vantage point (more on this later). Things can get complicated very quickly when trying to decipher EKGs, and the most important thing is to work through the information in a systematic process.
The first thing we must do is evaluate what we are hoping to actually see on the EKG. When looking at the typical image of a EKG (below) it is important to realize what each portion of the tracing represents physiologically.
P wave: is the first short upward movement of the EKG tracing. It indicates that the atria are contracting, pumping blood into the ventricles.
The QRS complex: normally beginning with a downward deflection (Q), a larger upwards deflection (R); and then a downwards S wave. The QRS complex represents ventricular depolarization and contraction.
T wave: is normally a modest upwards waveform representing ventricular repolarization.
U wave: is sometimes seen and marks re-polarization of the purkinje fibers.
CHEST/PRE-CORDIAL LEADS
One must think of these leads as “cameras” that take electrical snapshots of how the heart is function from different perspectives around the body. If the electrical signal is going towards the lead a positive line is seen on the EKG, and if the signal is going away from the lead this is seen as negative on the EKG. There are two sets of 6 leads (chest and limb leads) that are used to generate axis around the heart.
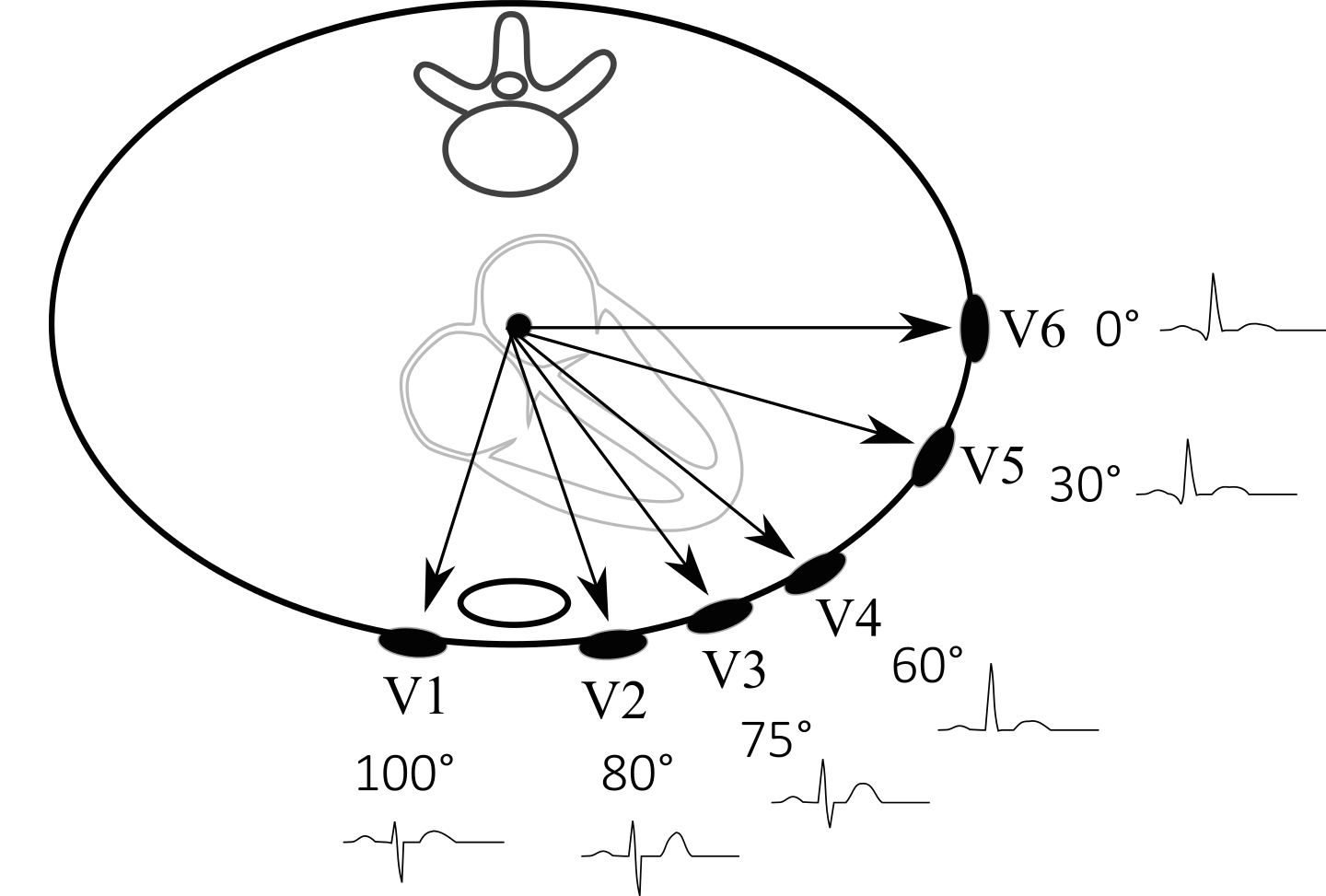
Chest/pre-coridal leads: these leads are arranged around the heart in an axial plane (think of a hula hoop around the chest). The leads are referred to as V1-V6 (see image below)
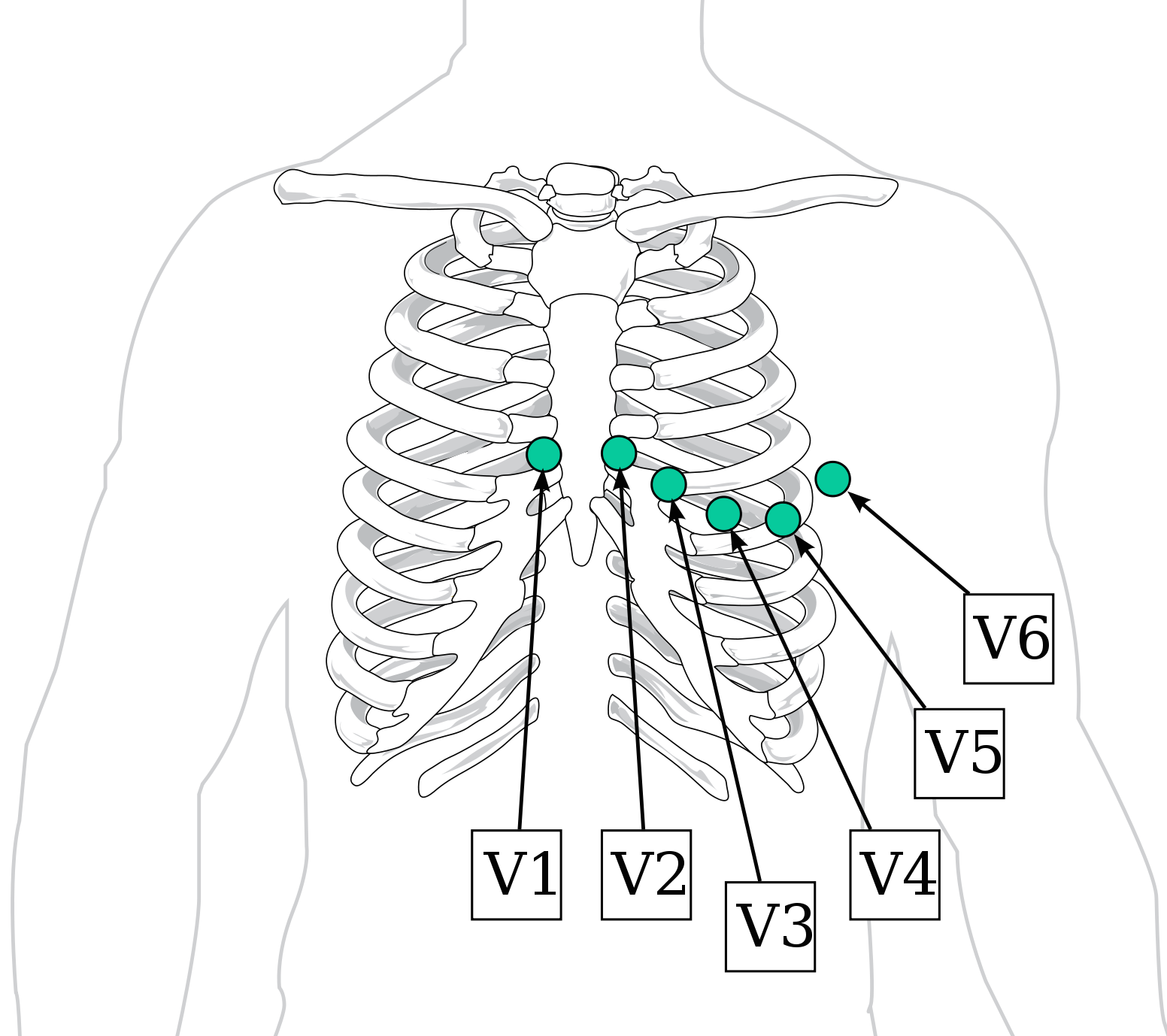
With the placement of these leads in mind, let us take a look at the position of the leads around the heart (below). Generally speaking leads next to the right side of the heart (i.e. V1) and leads next to the left side of the heart (i.e. V6) can be used to localize specific pathology (i.e. an enlarged left ventricle can increase the positivity of lead findings on leads such as V6 because more cardiac muscle is moving electrical activity towards that lead).
LIMB LEADS
The most important thing to keep in mind about these limb leads are that they form an axis around the heart that is perpendicular to the chest leads (if the chest leads are a hula hoop horizontally around the heart, the limb leads would be analogous to a vertical hula hoop that runs from the top to the bottom of the heart). Worrying about the specifics of each lead (i.e. which are unipolar vs. bipolar) is not terribly critical at this point, however keeping in mind their names and position (image below) is critical.
Generally speaking now we can appreciate the connection between leads and the inferior portion of the heart (II, III, AVF) , the right side of the heart (AVR), and the left side of the heart (AVL).
HEART RATE
Now that we know what the EKG is for, and where the leads are, now we can begin interpreting it. The first thing to do clinically (after checking that the EKG is for the patient you are seeing) is to determine the heart rate. There are multiple methods of doing this, however perhaps the most intuitive is to realize that the EKG generally is a 10 second strip (when looking at the leads reported at the bottom of the EKG) and we can multiple the number of QRS complexes in this 10 sec strip to obtain the number of heart beats per minute (see example below)
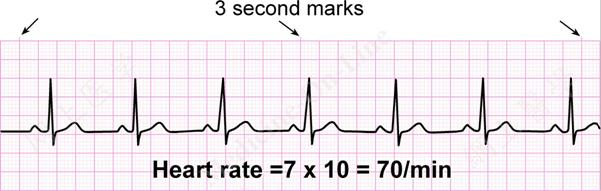
A few good numbers to keep in mind are the following:
- The speed of a typical EKG reading is 25 mm/sec.
- Each small box is 1 mm x 1 mm in size (width is 0.04 s)
- Each large box (5 small boxes per large box) is 5 mm x 5 mm in size (width is 0.20 s)
- There are 1500 little boxes in 1 min
- The heart rate (estimated from 2 points) will be: 1500/# of boxes between points
We will use this information later when looking at clinically relevant intervals.
SINUS RHYTHM
Sinus rhythm is a term that can get unnecessarily complicated. All it means is that the origin of the heart beat is beginning at the sinus node (which is of course normal). In order to determine if a patient has sinus rhythm, one must ask themselves a few questions.
- Are there P waves present? Looking at leads I, II, and III p waves should be visible if the heartbeat is beginning at the SA node. If there are no P waves, then the patient does not have sinus rhythm.
- Is the tracing positive in lead II? Anatomically, if the heartbeat begins at the SA node, it must be depolarizing toward lead II (making the tracing positive in this lead). If the tracing is negative in lead II the patient is not in sinus rhythm.
- Is the tracing negative in lead AVR? Given that this lead is directly opposite lead II, if the patient has sinus rhythm, this tracing should be negative.
After looking at heart rate it is important to characterize the rhythm of the heart. Sinus rhythm refers to any cardiac rhythm where depolarization of the cardiac muscle begins at the sinus node, as well as alternating atrial and ventricular contraction. It is characterized by the presence of correctly-oriented P waves on the electrocardiogram (ECG). Sinus rhythm is necessary, but not sufficient, for normal electrical activity within the heart. In addition to correct P waves, the below flowchart can be used to help characterize what sinus rhythm is.
***IT IS IMPORTANT TO REALIZE THAT THERE ARE MISINFORMED DEFINITIONS OF SINUS RHYTHM THAT INCLUDE EXTRA CRITERIA! Often you may hear/see additional criteria for sinus rhythm that require for a p wave to be present after every QRS complex (and vice versa). These are popular but misinformed definitions of sinus rhythm (because they literally have nothing to do with the origin of the beat at the SA node). Similarly, the leads discussed above are usually the only ones that one needs to look at to determine sinus rhythm (although some may try to convince you to look at others as well).
AXIS OF HEART’S ELECTRICAL ACTIVITY
After calculating the rate and the rhythm, we can determine the axis of the heart’s electoral activity (in essence, what direction is MOST of the heart’s electrical activity going). This also is an important clinical descriptor because it can help character underlying clinical biology (i.e. left ventricular hypertrophy can cause left axis deviation).
Based upon the specific positions of the limb leads (see below) we can help characterize the heart’s axis.
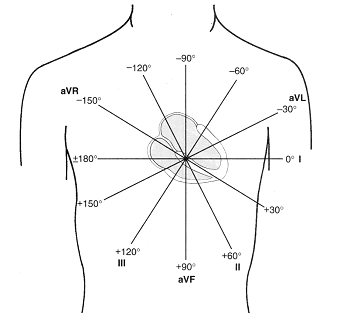
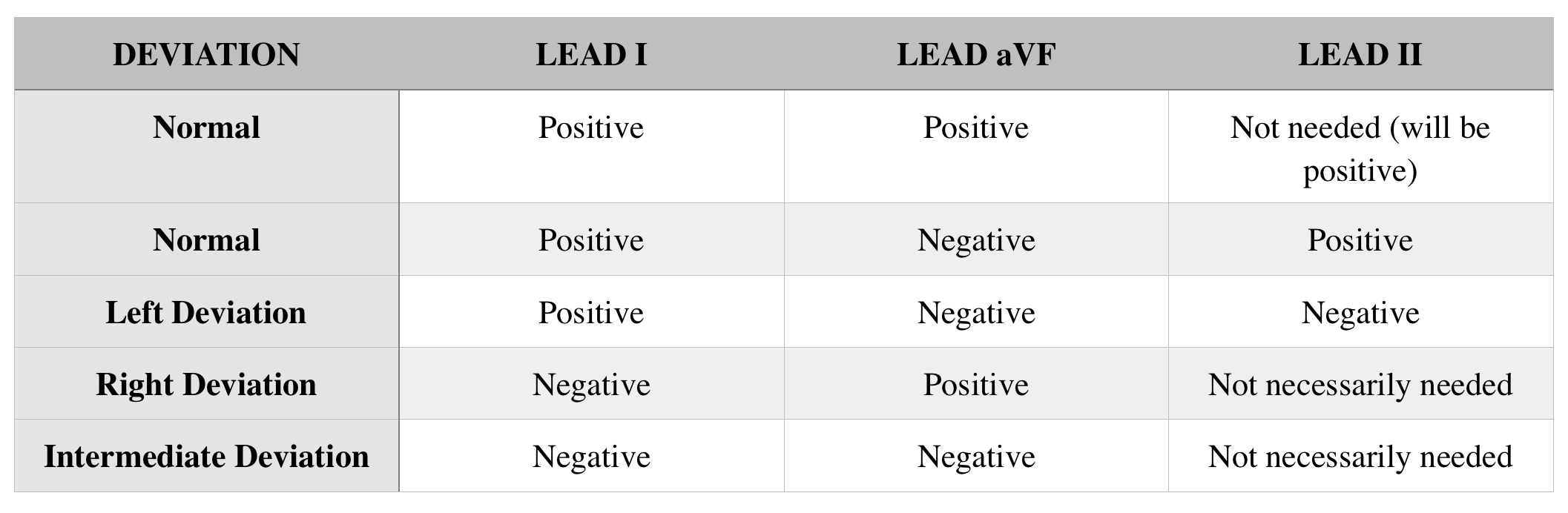
Lets keep in mind that lead I marks the 0° position on the left side of the heart, and AVF points towards the feet of the individual (and market the 90° position). The normal axis is from +90° to -30° with. The below is a quick summary of common lead findings and their respective heart deviations.
INTERVALS
After intercepting all of the above values/characteristics we now can start to delve deeper and characterize the nature of different intervals. Looking at any lead it is useful to characterize how wide the following intervals are: PR, QT, QRS (see image below).
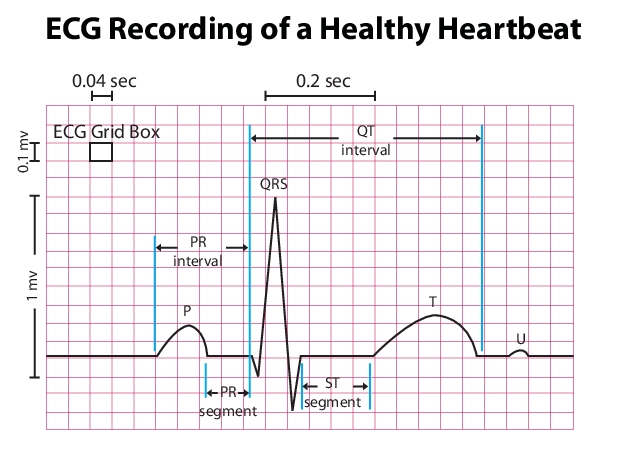
PR interval: time between the start of the P wave and the beginning of the QRS complex (start of atrial contraction to the start of ventricular contraction). Check to make sure this distance is larger then 3 small boxes (0.12 s) below the size of one big box (0.2 s). If it is longer then 0.2s, this is characterized as first degree AV block.
QRS interval: the time between the start and end of the QRS complex (i.e. the time of ventricular contraction). This should be less that 0.10 sec (~3 boxes). >100ms can represent a ventricular conduction abnormality (bundle branch block) or beats originating in the ventricular myocardium
QT interval: time between the start of the QRS complex and the end of the T wave (time between ventricular contraction and ventricular re-polarization). First calculate the time between the two subsequent R-R points (time between 2 ventricular contractions) and then make sure the QT interval is less than half this amount of time. Greater than half the RR interval is referred to as a prolonged QT.
MORPHOLOGY
Looking at all of the leads it is important to look and see if there are any notable morphological changes with the: P wave, QRS complex, ST segment, T wave.
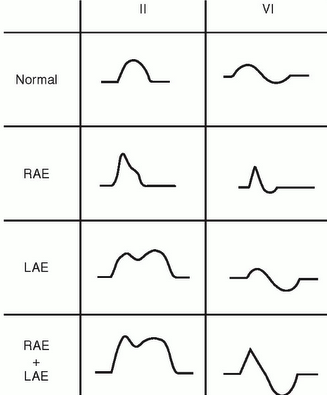
P wave: look at the size and shape of the P wave. Very prominent P waves are suggestive of atrial enlargement (V1 for left atrium, II for right atrium). Greater than 1 small box is a larger P wave that should be noted.
*In lead V1, the P wave can sometimes be split because of the differential direction between right atrial and left atrial enlargement (right atrium contracts first, and is positive in this lead, left atrium is second and is negative here). Different pathology can manifest in different types of P wave splitting in lead V1 vs. lead II (table below).
QRS complex: look at these in all the leads but pay special attendant to V1-V6. Check to see the shape and size of the peak. An enlarged peak is suggestive of increased mass of either the left or right ventricle (or both). While not important to memorize right now, keep in mind that there are guidelines for EKGs to help diagnose left or right ventricular hypertrophy.
ST SEGMENT ELEVATION
Before we discuss how ST segments are used clinically, we must first appreciate (and accept) that the specific reason why ST segments are modified is not fully understood. We understand associations and patterns, but don’t know the underlying biology/physiology. For our purposes, lets just keep in mind that if we were to find an abnormal ST segment on an EKG we would have other tools at our disposal (imaging, patient history, etc.) that we would use to help characterize the underlying pathology behind the EKG finding.
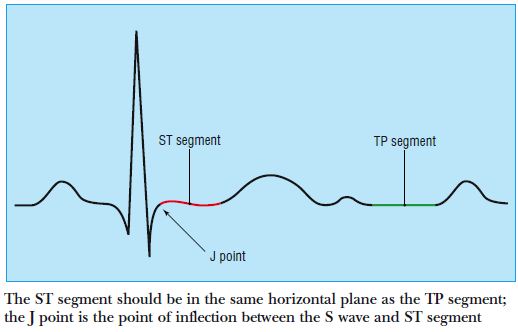
With this in mind, let us discuss the clinical utility of both ST segment elevation, as well as ST segment depression. As a reference we use the TP segment (seen below) to distinguish if the ST segment is elevated or depressed (these normally should be at the same level).
ST segment elevation: generally speaking, elevated ST segments are very suggestion of myocardial infarction (MI). When we see ST elevation we are concerned about an MI in the associated region/artery. This trumps all other concerns given how serious this finding is.
Given that an MI change depending on how long it has been occurring, the below image gives one representation of its progression. Actual EKG findings can be variable.
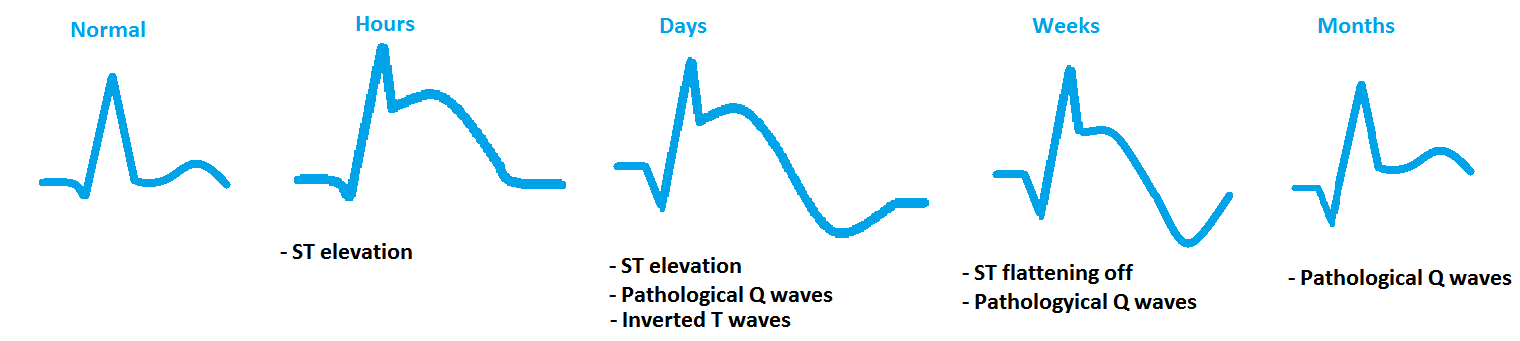
Let us pay special attention to the pathological Q waves that can be seen post MI. These waves develop/become more prominent because cardiac tissue that was responsible for causing positive deflections in certain leads has died/is no longer present.
Localization of leads to arterial territories: While never a 100% trend, the presence of ST elevation in certain leads can indicate the likely source of infarction. Here are some major associations that are useful to keep in mind (that might change your clinical eye after reading an EKG). Lets first remind ourselves of the major cardiac arteries: Left anterior descending (LAD), left circumflex (LCx), and the right coronary artery (RCA).
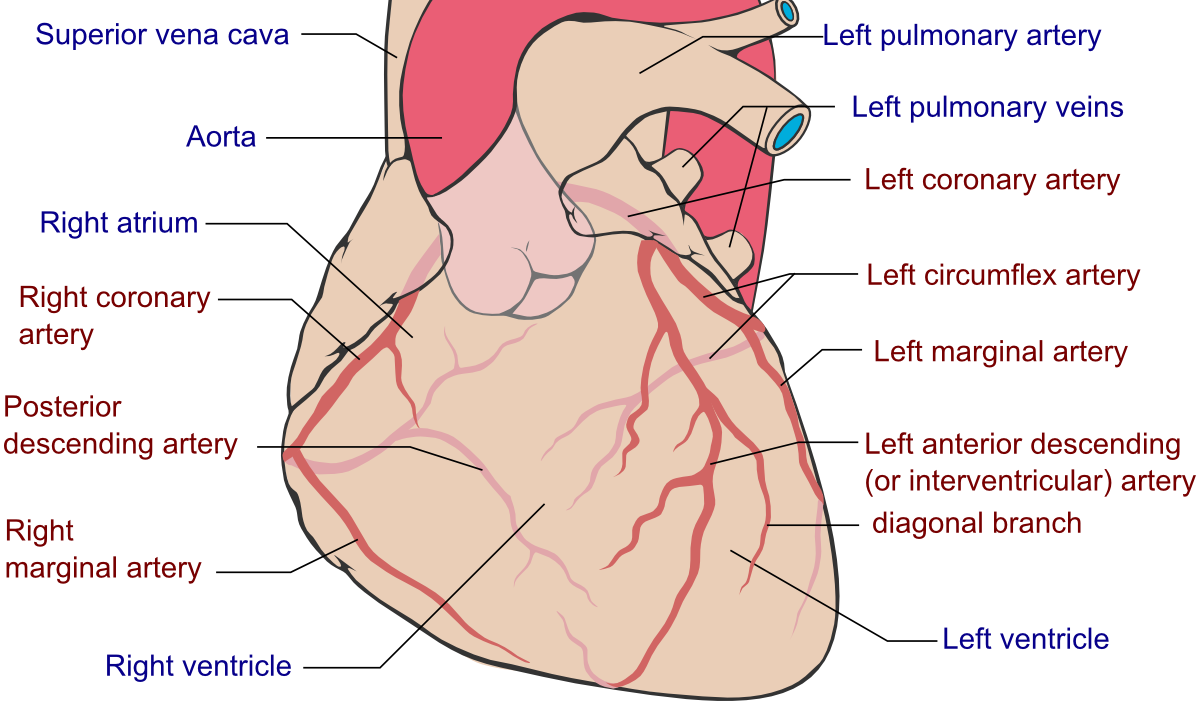
With the cardiac artery in mind, here are the associations to make sure you remember:
Leads V1, V2: LAD anteroseptal
Leads V3,V4: LAD anteroapical
Leads V5,V6, I, aVL: LCx
Leads II,III, aVF: RCA
*the location of these leads combined with the anatomical location of the arteries helps us associate them together. Remember these associations not just by memorizing but rather by working through where leads are with respect to the major cardiac arteries.
ST SEGMENT DEPRESSION
While a lot of similarities exist between our approach to analyzing/localizing ST segment depression, these are usually less serious and can often times indicate ischemia vs. a more severe infarction. Below is an example of a EKG finding.
*sometimes an ST elevation in the lateral leads (such as lead I) can cause a depression in the inferior leads (such as aVF) simply because the direction of the electrical activity is going in an opposite direction. Always worry about the ST elevations first!
T WAVES
Generally T waves should be in the same direction of the QRS complex. If they are not there could be an underlying issue (such as ischemia) in the territories of that lead. Look at size and whether or not they are inverted (as seen below).

ATRIAL/VENTRICULAR BLOCK (AV BLOCK)
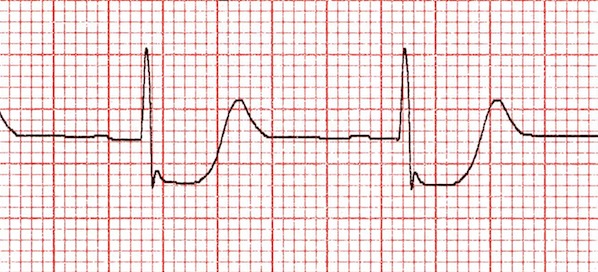
Quite simply, AV block refers to impaired conduction between the atria and ventricles of the heart (P waves and QRS complexes respectively) . There are a number of different types of AV block that are discussed below.
1st degree AV block: this is simply an increase in the PR interval (greater than 5 boxes/0.20 secs). This is not typically thought to be pathological, and is a common EKG finding.

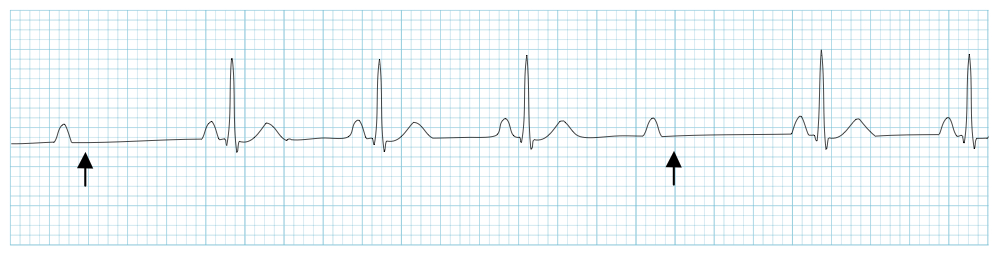
2nd degree AV block: there are two different types which different in there characteristics.
Mobitz 1, Wenckebach: the PR interval progressively increases until a QRS complex is skipped (and the pattern begins to repeat itself).
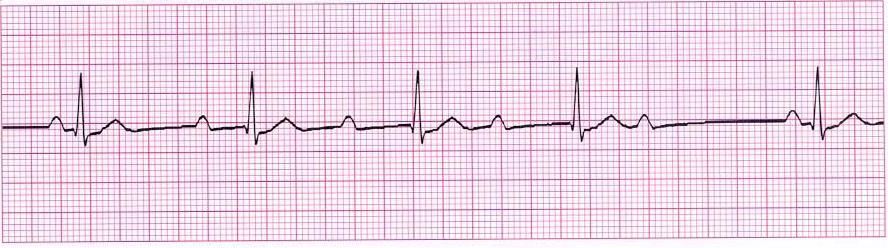
Mobitz 2, Hay: PR interval remains unchanged however periodically there is failed ventricular contraction. This is a more serious condition than Mobitz 1 AV block.
3rd degree AV block: there is no association between P and QRS complexes at all and these contract independently of each other (the atrial and ventricular contractions have become separated from one another).

BUNDLE BRANCH BLOCKS (BBB)
Interruption of conduction through the right/left bundle branches may develop from damage (ischemic or degenerative). The affected ventricle will not depolarize in the normal sequence as a result. Rather than rapid uniform stimulation by the Purkinje fibers, the cells of that ventricle must rely on relatively slow cell to cell (myocyte-to-myocyte) spread of electrical activity traveling from the unaffected ventricle. This delayed process prolongs depolarization and widens the QRS complex. Remember that a normal QRS duration is ?0.10 sec (?2.5 small boxes).
***A QUICK WAY TO DETERMINE RIGHT VS LEFT BBB is to look at the V1 lead. If V1 is positive, it is most likely a right BBB. If V1 is negative, it is most likely a left BBB.
Right bundle branch blocks: patients will have impaired conducting though the right ventricle of the heart (however the septum conduction will be intact given that this is controlled by the left side of the heart). Widened QRS complexes can be seen, and a prominent RSR’ complex in V1, and a prominent S wave in V6.
R’ complex: this is a positive deflection on the EKG found after the QRS complex due to the delayed contraction of the right side of the heart (it is not hidden by the S wave which normally occurs).
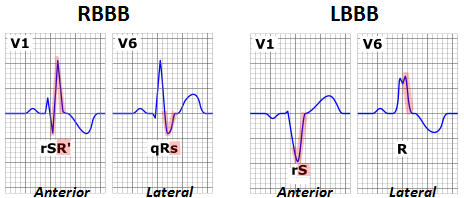
Left bundle branch blocks: this produces even more abnormal QRS findings simply because the septum does not depolarize. One can appreciate a broadened QRS, absent R/prominent S on V1, and a broad notched R in V6.
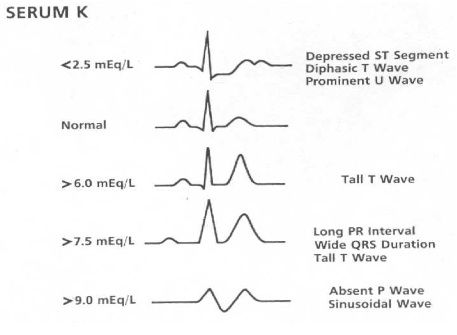
POTASSIUM ABNORMALITIES
ATRIAL FIBRILLATION
ATRIAL FLUTTER
Page updated: 05.17.16