Page Contents
OVERVIEW
This page is dedicated to covering the approach to a patient who presents with post menopausal bleeding.
WHAT IS POST MENOPAUSAL BLEEDING?
Postmenopausal bleeding (PMB) often refers to vaginal bleeding that is experienced by a post menopausal woman (who has not experienced menstruation for at least 12 months).
More restrictive definition: Some individuals use a more restrictive definition of PMB that refers to patients who only have uterine bleeding and are not on hormone therapy.
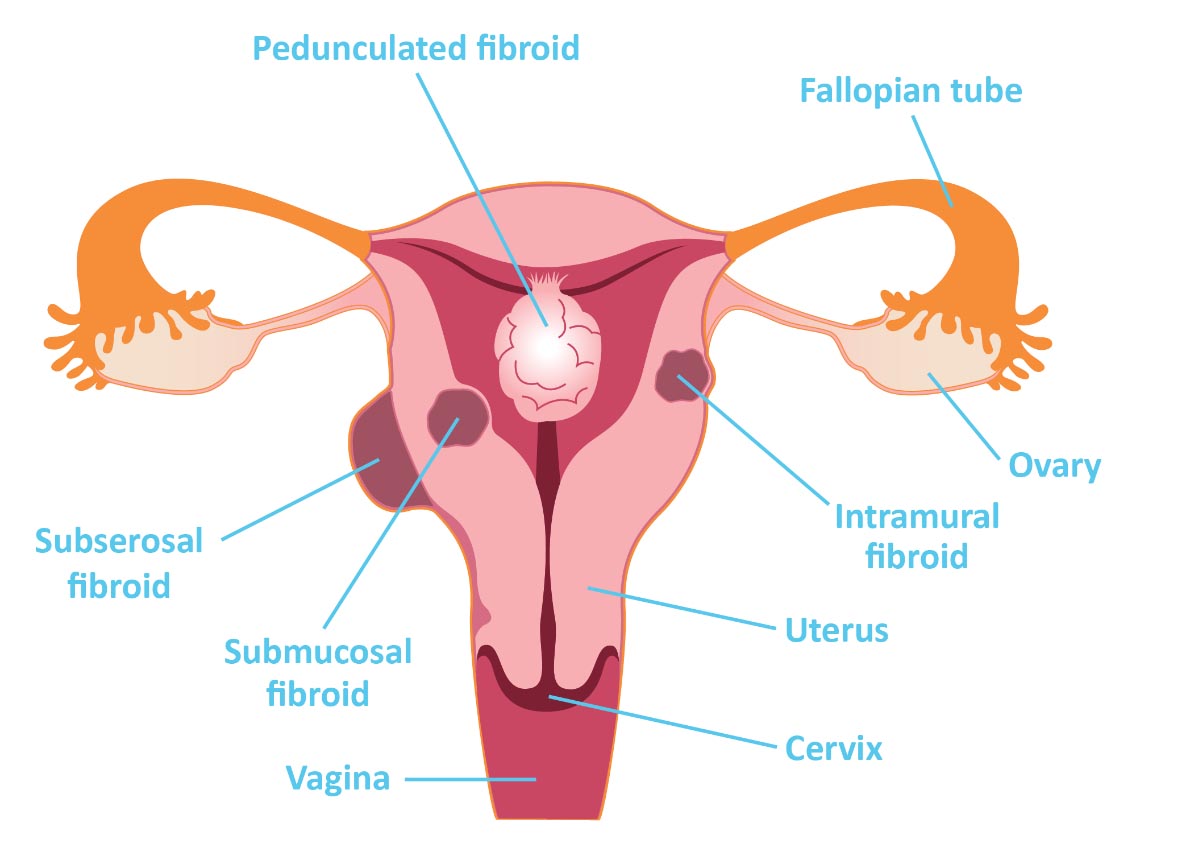
It is important to appreciate that abnormal bleeding noted in the genital area is often attributed to intrauterine bleeding, but actually may be caused by bleeding from the cervix, vagina, vulva, or fallopian tubes, or be related to ovarian pathology. Other nongynecologic sites may also be the source of the bleeding (that can include the urethra, bladder, anus/rectum/bowel, or even the perineum).
*It is important to localize the source of the bleeding in the patient whenever possible.
WHAT CAN BE CAUSES OF PMB?
There are a few major categories of disease processes that can be the cause of PMB:
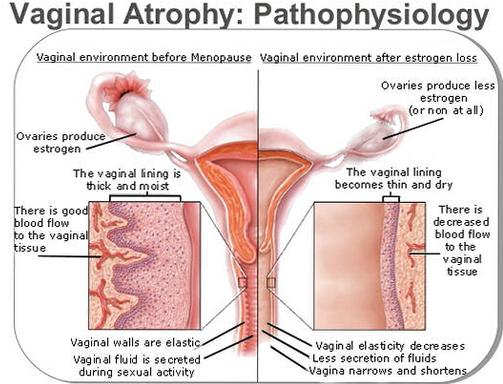
Atrophy: the most common cause of PMB is due to the atrophy of the uterus/vagina. Loss of estrogen signaling will result in atrophy of the endometrium and vagina. Internally this atrophied endometrium is prone to friction induced micro-abrasions that can result in vaginal bleeding. While common, this should not be assumed to be the cause of PMB!
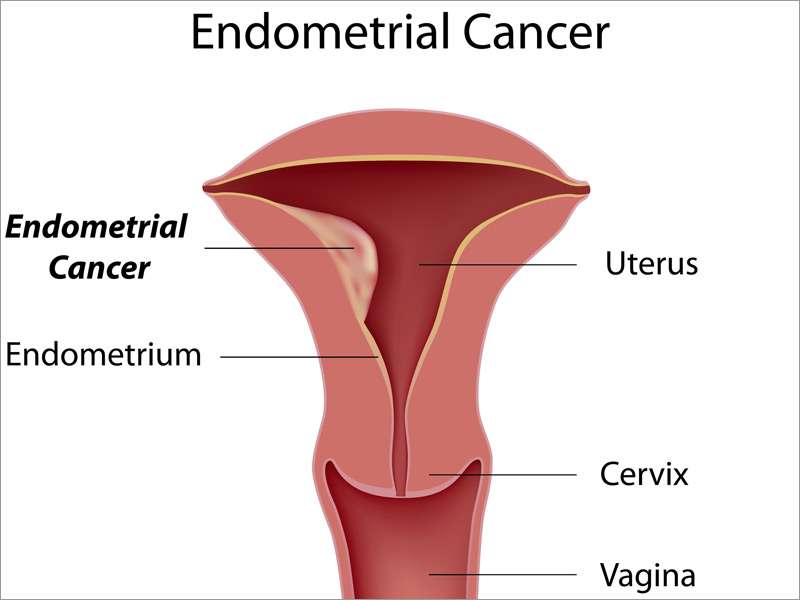
Malignancy: perhaps the most serious and dangerous cause of PMB, malignancy is an important diagnosis that must be explored in women with PMB. Endometrial cancer should likely be evaluated in all patients who have PMB. Cervical cancer is also a possible cause of vaginal bleeding.
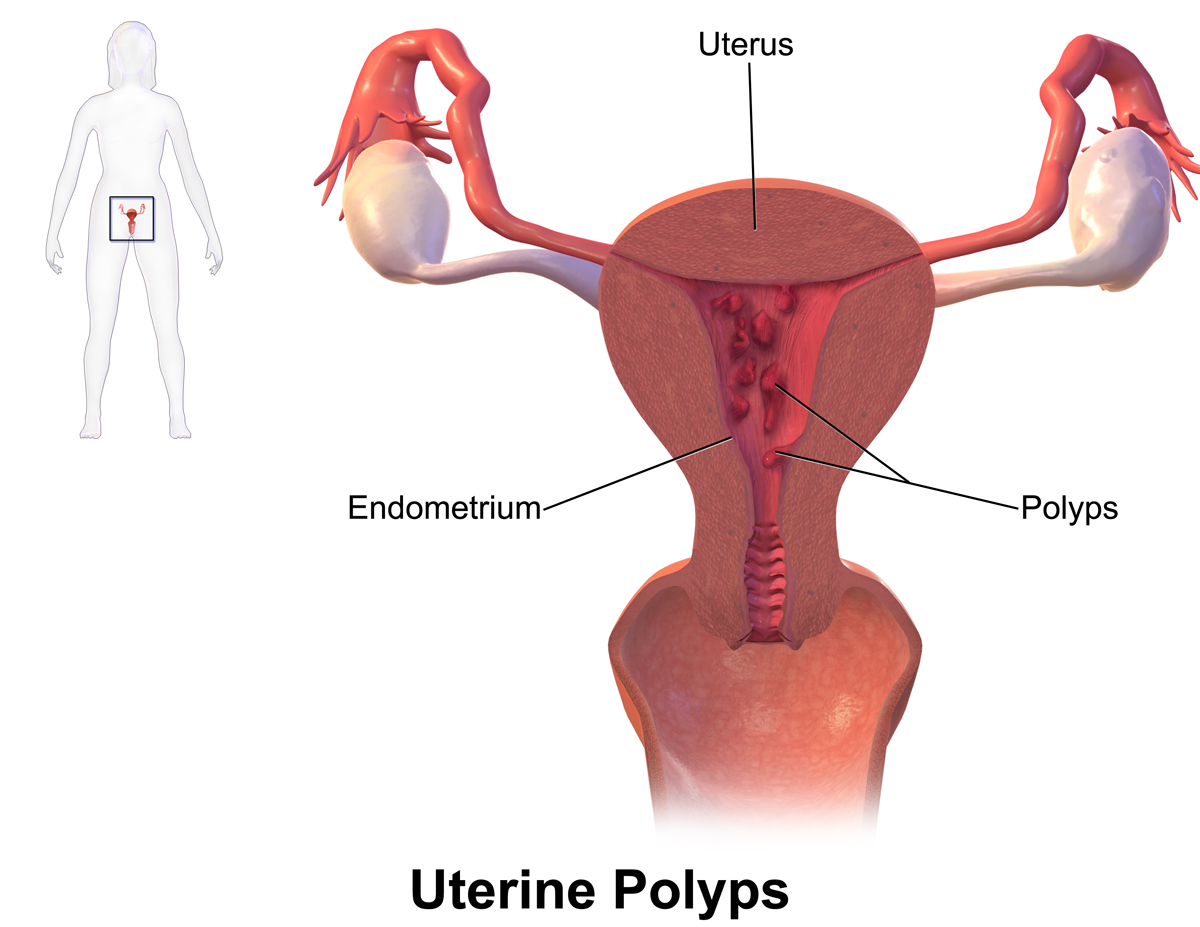
Polyps: being endometrial/cervical polyps may also be the cause of uterine bleeding after menopause, and are not uncommon.
Exogenous estrogens: hormone therapy/exogenous sources of estrogens can be a common cause of uterine bleeding in patients who are post-menopausal (and it is of course not uncommon for some post-menopausal women to be taking hormone therapy).

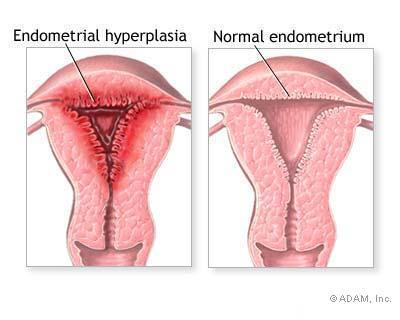
Endometrial hyperplasia (endogenous estrogens): clinically this can present with uterine bleeding. It is important to note however that given the nature of menopause, there must be a source of estrogen that is responsible for causing the growth of the endometrium. Endogenous estrogen production from ovarian or adrenal tumors or exogenous estrogen therapy can be a possible causes. Similarly obese women also have high levels of endogenous estrogen due to the conversion of androstenedione to estrone and the aromatization of androgens to estradiol, both of which occur in adipose tissue throughout the body.
Leiomyomata uteri (fibroids) are the most common pelvic tumors in women, and occasionally can be cause of PMB in patients. With this in mind uterine sarcoma should be considered in postmenopausal women with presumed uterine leiomyomas producing their symptoms.
Other causes: the above list is by no means exhaustive, however does cover some of the major categories of processes that can cause PMB. Other causes can include: infections, adenomyosis, damage to surrounding organs, post radiation therapy, large doses of soy products, and anticoagulant therapy.
HOW DO PATIENTS WITH PMB PRESENT?
Given the nature of PMB, patients who present with it will be older women that complain of vaginal (or suspected vaginal bleeding). Patients might notice spotting on their underwear, blood in their urine, or may even begin to use pads/tampons again to combat vaginal bleeding.
GATHERING HISTORY FOR PATIENTS WITH SUSPECTED PMB
While by no means a full list of questions, one of the first steps during a patient encounter is gathering the patients medical history so there are a few important elements that are worth investigating when meeting a patient with PMB.
Last menstrual period? while very obvious, it is of course important to make sure that the patient is actually post menopausal by asking them when exactly their last menstrual period was.
Where is the bleeding is coming from? while this will be further explored with the physical exam later, the patient can characterize if the bleeding is actually coming from the vagina (vs. the anus/perineum/etc). It is important to realize that spotting on underwear/pad doesn’t necessarily mean the bleeding is from the vagina. Patients can be asked if there is any blood on toilet paper when they wipe to further investigate if there is bleeding outside the vagina.

When is the bleeding occurring? While difficult to definitively localize the exact anatomical source of the vaginal bleeding, one must appreciate that if the bleeding is only from the patient’s bladder (not a cause of PMB) it might only occur during urination.
Current medications being taken? It is important to see if the patient is taking any hormone therapy, anticoagulants, or even supplements (such as soy products) that might be causing/contributing to the bleeding.
PHYSICAL EXAMINATION OF PATIENT WITH SUSPECTED PMB
While of course a full gynecological exam should be conducted whenever possible, there are a few components of the physical exam that are relevant to patients with PMB that are highlighted below.
Any visible bleeding: while perhaps an obvious statement, but throughout the exam careful note of any locations of obvious bleeding/trauma should be taken. Areas to pay interest to include:
- Anus
- Perineum
- Vaginal canal
- Cervix
Sings of bleeding outside of the vagina suggest a process that is unrelated to PMB.

Sings of vaginal atrophy: when examining the vagina there are some clear signs vaginal atrophy. These classical sings include a pale, dry vaginal epithelium that is smooth and shiny with loss of some rugation. While not diagnostic on its own, this can be more suggestive of processes such as atrophy contributing to/causing PMB.
DIAGNOSTIC TESTING PATHWAY FOR PMB
In the absence of an obvious cause of PMB/suspected PMB, a clear diagnostic pathway can be taken so that no important diagnoses are missed. Below are some important tests (in roughly the order they often can be conducted in):
Endometrial biopsy: histological evaluation of the endometrium is an important step in working up a patient with PMB. It can help assess for atrophy, endometrial cancer, hyperplasia, or other histological abnormalities that can cause PMB. This is often one of the first steps.
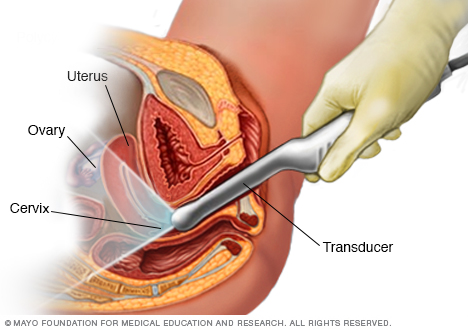
Transvaginal ultrasound: this imaging technique can be used in patients who require in evaluation for uterine pathology (eg, polyp, leiomyoma) or for adnexa pathology. Patients who also can not tolerate endometrial biopsy can also have this technique used for endometrial analysis.
Cervical cytology can be conducted to assess for possibility of cervical cancer.
Cervical biopsy of any suspicious lesions on the cervix can help investigate and diagnosis cervical cancer.
Page Updated: 06.18.2016