Page Contents
- 1 WHAT IS IT?
- 2 WHY IS IT A PROBLEM?
- 3 WHAT MAKES US SUSPECT IT?
- 4 HOW DO WE CONFIRM A DIAGNOSIS?
- 5 HOW DO WE RULE OTHER DIAGNOSES OUT?
- 6 HOW DO WE TREAT IT?
- 7 HOW WELL DO THE PATIENTS DO?
- 8 WAS THERE A WAY TO PREVENT IT?
- 9 WHAT ELSE ARE WE WORRIED ABOUT?
- 10 OTHER HY FACTS?
- 11 ARCHIVE OF STANDARDIZED EXAM QUESTIONS
- 12 FURTHER READING
WHAT IS IT?
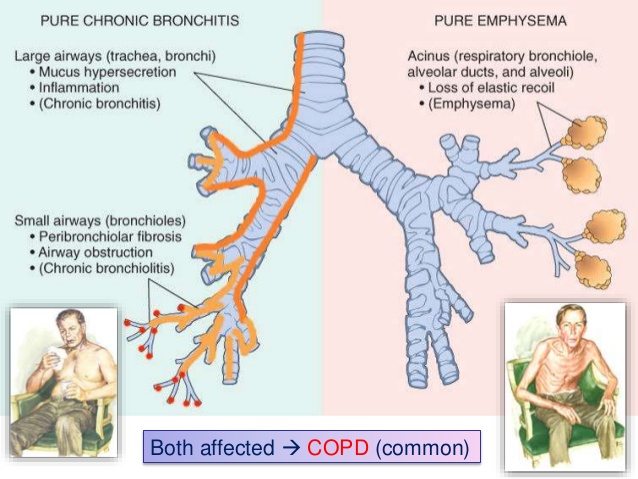
Chronic Obstructive Pulmonary Disease (COPD) refers to lung condition that (as the name suggests) falls into the category of “obstructive lung diseases”. There are two major subtypes of COPD (both of which are typically exhibited by patients, so while irrelevant for clinic this is testable for STEP 1):
- Chronic bronchitis: defined as a productive cough lasting at least 3 months (given a period of 2 years). Mucus glands are hypertrophied and hyper secrete mucous leading to obstruction within the airways. These patients typically are hypercapnic (mucus plugs retain CO2), and become both hyperemic and cyanotic earlier in their disease course.
- Emphysema: destruction of alveolar wall and elastic tissues surrounding alveoli are the cause of this subtype. Because of the pathophysiology, these patients have increased lung compliance and decreased lung elasticity. Furthermore, the loss of elastic tissues will lead to premature airway collapse (limiting airflow in patients during expiration).
WHY IS IT A PROBLEM?
Regardless of the subtype, COPD is fundamentally characterized by both chronic airflow limitation and obstruction (that is NOT fully reversible). Patients simply are not able to expire all of their inhaled air upon breathing out. This is because airway obstruction and premature airway closure block the path of expired air leading to hyperinflation in the lungs. This hyperinflation (over time) will lead to a decreased ability to inspire sufficient volumes of air on subsequent breaths, leading to decreased delivery of oxygen to the lungs and the blood (causing decreased O2 saturation levels).
WHAT MAKES US SUSPECT IT?
Risk Factors:
Cigarette smoking (BIGGEST RISK FACTOR)
Initial Presentation:
- Dyspnea is a common chief complaint among patients
- Persistent cough
- Sputum production
History Of Present Illness:
Age of onset is generally in those 45 years or older
Physical Exam:
Vitals: decreased oxygen saturation can be observed in patients with more severe COPD.
Respiratory exam:
- Productive cough may be heard/observed in patients
- Use of accessory muscles for respiration
- Barrel chest upon visual inspection can suggest hyperinflation in a patient.
- Wheezing can be heard on auscultation
- Decreased breath sounds may also be appreciated on auscultation

Dermatological exam:
- Cyanosis of the skin, lips, tongue, nails, and mucous membranes can be preset
HOW DO WE CONFIRM A DIAGNOSIS?
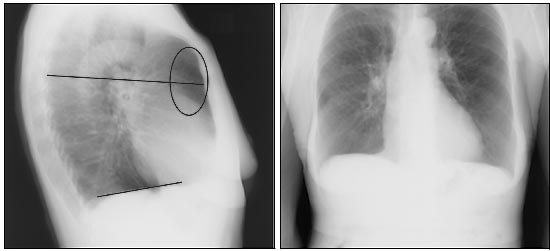
Chest X-ray can demonstrate:
- Hyperexpanded-hyperlucent lung fields
- Flattened hemidiaphrams (given hyperinflation of lungs)
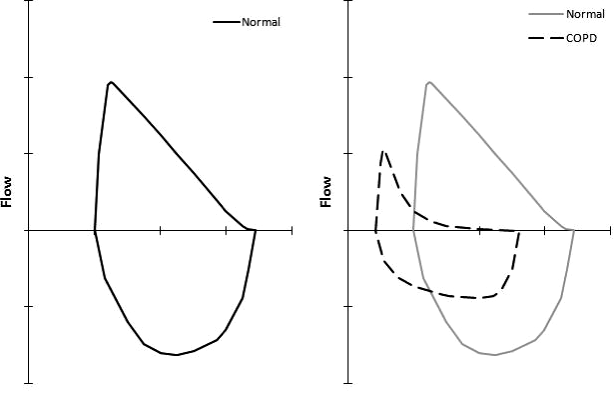
Pulmonary Function Tests (PFTs) often reveal the following findings:
- Increased total lung capacity (TLC)
- Increased residual volume (RV)
- Decreased forced expiratory volume in 1 second (FEV1)
- Decreased forced vital capacity (FVC)
- Reduced FEV1/FVC ratio: while both FEV1 and FVC are typically decreased in COPD, FEV1 is usually decreased to a larger extent (shrinking this ratio). A FEV1/FVC ratio less than 0.7 is used to diagnose COPD (source).
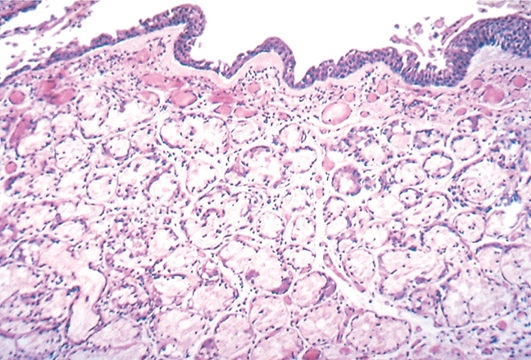
Mucus gland hypertrophy can be characterized histologocially in chronic bronchitis using something called the Reid index (ratio of mucous gland depth relative to the thickness of bronchial wall). Reid index typically increases above 50% in chronic bronchitis (normal below 40%).
HOW DO WE RULE OTHER DIAGNOSES OUT?
Pulmonary function tests ultimately will help distinguish COPD from other lung diseases. Restrictive lung diseases will not have an elevated residual volume as is the case with COPD. Asthma while similar to COPD in many ways, typically is reversible with the administration of short acting bronchodilators (PFTs will return to normal after administration) while COPD typically is not very responsive to this therapy (and is not a reversible condition).
HOW DO WE TREAT IT?
For more detailed information, read the page dedicated to the topic of treating patients with COPD.
Lifestyle changes:
*Smoking cessation is a key treatment for most all patients with COPD (if the patient in question is currently a smoker).
Medical Management:
Muscarinic antagonists (such as Ipratropium, tiotropium) will antagonize ACh signaling (leading to bronchodilation).
- Ipratropium completely blocks muscarinic receptors (preventing bronchoconstriction).
- Tiotropium is similar however is longer acting.
Beta 2 Agonists (such as albuterol, salmeterol) will cause bronchodilation. These also agonize beta 1 receptors (but to a lesser extent).
Inhaled corticosteroids can also be used in some patients (this will decrease chance of exacerbation, but increases infection risk).
Other:
Supplemental oxygen should be given to patients that have resting hypoxemia (PaO2 ≤ 55 mm Hg or oxygen saturation ≤ 88%)
HOW WELL DO THE PATIENTS DO?
COPD is not a reversible condition, is typically progressive, and dyspnea will be persistent in patients. Mortality depend on the stage of COPD, however is overall high for patients with this condition.
WAS THERE A WAY TO PREVENT IT?
Avoiding smoking could help prevent many cases of COPD.
WHAT ELSE ARE WE WORRIED ABOUT?
Secondary spontaneous pneumothorax can commonly be caused by COPD
Pulmonary hypertension can be cased by COPD (due to the destruction of the lung parenchyma). This can lead to the failure of the right ventricle which is called for pulmonlae (in the absence of left heart failure).
Infectious exacerbations of COPD can be common (and can present as pneumonia). Some common pathogens are:
- Hemophilius influenzae
- Moraxella catarrhalis
- Legionella pneumophila
Alpha-1 antitrypsin (A1AT) deficiency: panacinar emphysema is associated with this enzyme deficiency (as is liver cirrhosis). This is a genetic condition that results in the lack of activity of A1AT (an enzyme responsible for inhibiting many proteases). In the absence of A1AT activity, proteases like neutrophil elastase can destroy structures within the lungs (such as elastase) leading to emphysema.
OTHER HY FACTS?
Giving patients cholinomimetic agents can exacerbate COPD (given role of ACh in the respiratory tracts)
Beta blockers can exacerbate asthma/COPD if given in excess
Blue bloaters can refer to COPD patients (chronic bronchitis subtype usually) who are obese and cyanotic.
ARCHIVE OF STANDARDIZED EXAM QUESTIONS
This archive compiles standardized exam questions that relate to this topic.
FURTHER READING
Page Updated: 04.04.2016