Page Contents
OVERVIEW
This page is dedicated to covering a very important call case: perforated appendicitis. This page will specifically cover this diagnosis in the setting of making the finding on abdomen/pelvis CT imaging.

Many of the cases presented here will be CT scans of the abdomen/pelvis with contrast however certain cases may present non-contrast imaging (which can have overlapping findings). This page assumes that you are familiar with acute uncomplicated appendicitis (which has a separate linked page).
WHAT IS IT EXACTLY?
Perforated appendicitis is a fairly self descriptive condition: it is acute appendicitis that has perforated (often times spilling fluid/gas into the abdomen).
WHY IS IT AN IMPORTANT CALL CASE?
As discussed on the acute uncomplicated appendicitis, appendicitis is generally a condition that has immediate surgical considerations (as many patients get an emergent appendectomy as well as antibiotics).
Noting perforation (by imaging) is important on call (and in general) as it can have implications on management:
- Surgical planning: if the patient will go for an appendectomy, knowing there is likely/definite perforation will help the surgeons plan their case.
- Delay surgery: in some cases, patients may be initially treated with antibiotics alone, and then return weeks/months later to have an interval appendectomy (to avoid operating when the abdomen is inflamed/irritated).
- Alter antibiotic course: patients with perforation generally will require a longer antibiotic course for treatment (given the extent of infection)
- Raise possibility of abscess formation: in general patients who have perforation will be at increased risk for developing an intra-abdominal abscess. This entity is discussed on the specific page for appendicitis complicated by absces.
In the end while it may seem like a subtle point, the presence of perforation (as detected on imaging) is clinically impactful in a number of ways, and makes perforated appendicitis a distinct entity.
WHAT CLINICAL CONTEXT HELPS RAISE SUSPICION FOR THIS DIAGNOSIS?
Patients may present in a manner very similar to those that have acute uncomplicated appendicitis. With that in mind there are some clinical clues that could suggest that a patient is perforated. It is important to note that perforation may present differently depending on how long the patient has been perforated however the timing of perforation is very challenging to definitely prove!
- Reported relief from abdominal pain: patients who acutely perforate often feel a period of pain relief (as obstructive process in the appendix is acutely decompressed).
- Worsening abdominal pain: while perforation may initially cause some relief, if it is left untreated patients will develop markedly worsening abdominal pain as they become peritonitic/septic.
- Physical exam: some patients may have rebound tenderness/peritonitis (more common in patients who have been perforated for some time).
- Unstable vitals: while not a requirement, some patients may present with vital signs (tachycardia, hypotension) which may reflect a sepsis type physiology. This can be seen in patients who have perforated for some time and have developed a more systemic response to disseminated infection.
WHAT IS THE KEY TO MAKING THIS DIAGNOSIS ON CALL?
The initial step is to identify if the patient has acute appendicitis which is covered in detail on the separate page on acute uncomplicated appendicitis.
Onc an appendicitis is identified, it is important to evaluate for clues to suggest perforation.
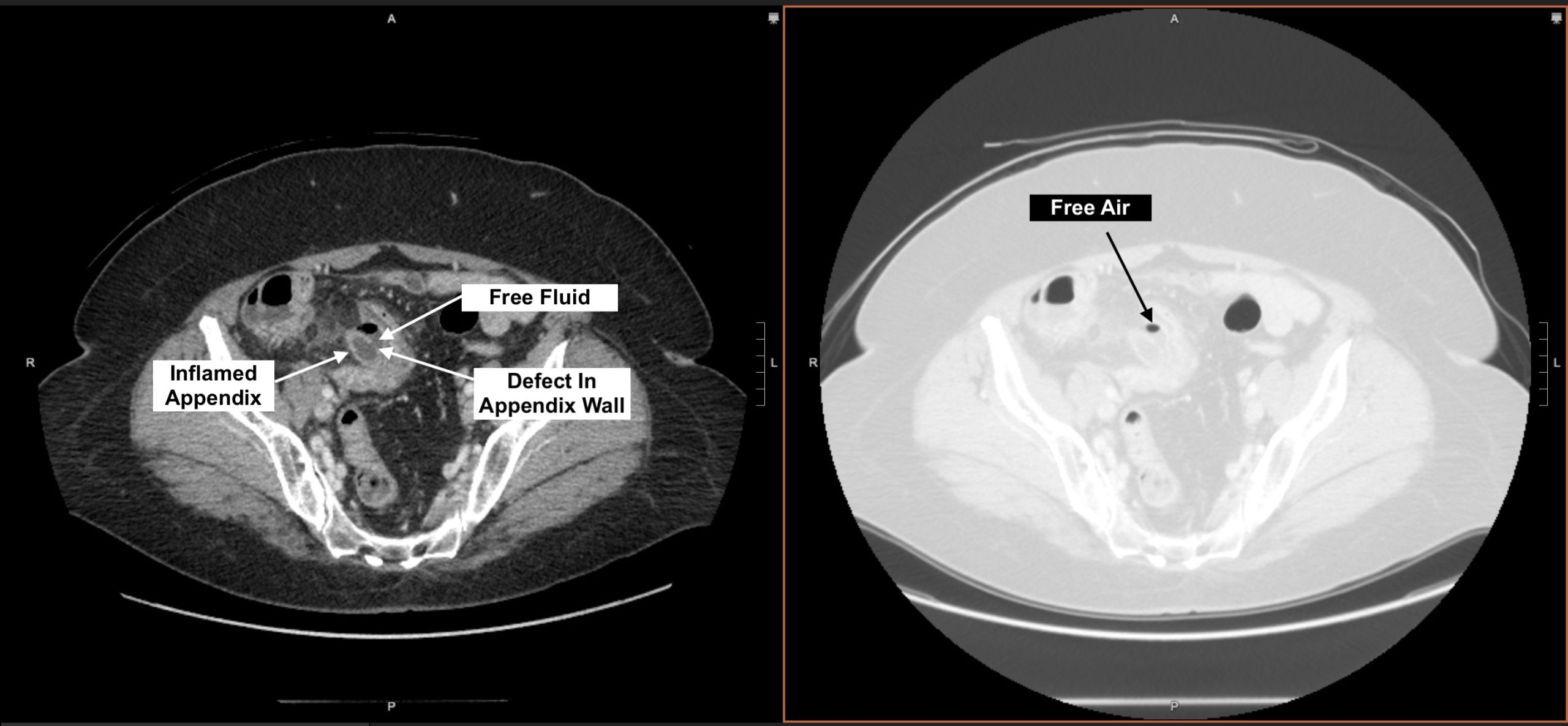
Characteristic imaging signs of perforated appendicitis include:
- Non-enhancing appendix wall/appendix wall defect: in some cases you will be able to identify the site of perforation by seeing the defect in the appendix wall.
- Free air: in cases of appendicitis with free air in the abdomen, the possibility of perforation is quite high. Make sure to use your lung windows to look for intra-abdominal free air!
- Free fluid: on its own, this may not suggest perforation (as free fluid can be reactive to acute uncomplicated appendicitis), however in combination with the above findings this can be suggestive of perforation.
- Special instance (missing base of the appendix): in some cases the appendix may rupture at its base and the connection between the cecum and the appendix may not be obvious. In these cases sometimes the distal appendix appears normal however don’t be fooled! Even if a long segment of the distal appendix appears normal this doesn’t exclude the possibility of a perforated appendicitis (if the base is indistinct etc).
WHAT HAPPENS NEXT AFTER THE DIAGNOSIS IS MADE?
As stated above, after this diagnosis is made patients will get some combination of antibiotics and surgery (although the timeframe may vary).
CASE ARCHIVE
Use the following login information to access the case archives: USERNAME: user, PASSWORD: password.
Click here to open up a case archive of perforated appendicitis seen on CT.
Page Updated: 02.16.23