Page Contents
OVERVIEW
This page is dedicated to covering a very important call case that is seen on call: an acute subdural hematoma. This is a category of intracranial hemorrhage that is often seen on non-contrast head imaging, however sometimes it can be difficult to appreciate given its location/proximity to adjacent bone.
This page will mainly focus on non-contrast head CT findings.
WHAT IS IT EXACTLY?
An acute subdural hematoma refers to blood products that are present between the meningeal layers of thee brain, specifically under the dura and above the arachnoid matter.
WHY IS IT AN IMPORTANT CALL CASE?
Any intracranial blood products are crucial to identify on call for a number of reasons. This includes (but is not limited to) the following considerations:
- Patients with any intracranial hemorrhage need to be closely observed: If a subdural hematoma is the only sign of bleeding and it is missed, patients may incorrectly be discharged from the hospital.
- Patients with intracranial hemorrhage often should not be anti-coagulated: this decision can become nuanced, but often the presence of intracranial bleeding (even a small subdural) informs a patient’s anticoagulation management (so as not to exacerbate the bleed).
- Subdural hematomas can cause significant mass effect: if a subdural bleed enlarges enough it can cause significant mass effect and even herniation. A subdural hematoma can be (or quickly become) a neurosurgical emergency.
WHAT CLINICAL CONTEXT HELPS RAISE SUSPICION FOR THIS DIAGNOSIS?
Patients may present with a few clinical context clues, however many of them are not always sensitive or specific for this diagnosis. Common presentations include:
- Trauma: acute or subacute traumatic injuries (such as a fall with a head-strike) are perhpas one of the most common scenarios
- Altered mental status: this can occur in a variety of contexts (trauma, recent anticoagulation initiation, with other neuro deficits in the setting of a subdural causing mass effect).
WHAT IS THE KEY TO MAKING THIS DIAGNOSIS ON CALL?
While large subdural hematomas are easy to detect on imaging, smaller ones can be very subtle. Also there there can be nuance regarding the density of the hematoma and its acuity. Here are some things to keep in mind when evaluating for subdural hematomas.
How to Detect Small “Hidden” Subdural Hematomas:
The proximity and density of the skull adjacent to the subdural space often times can make detecting a subdural hematoma veyr challenging. Here is what on should keep in mind to improve the chances of detecting a subdural hematoma.
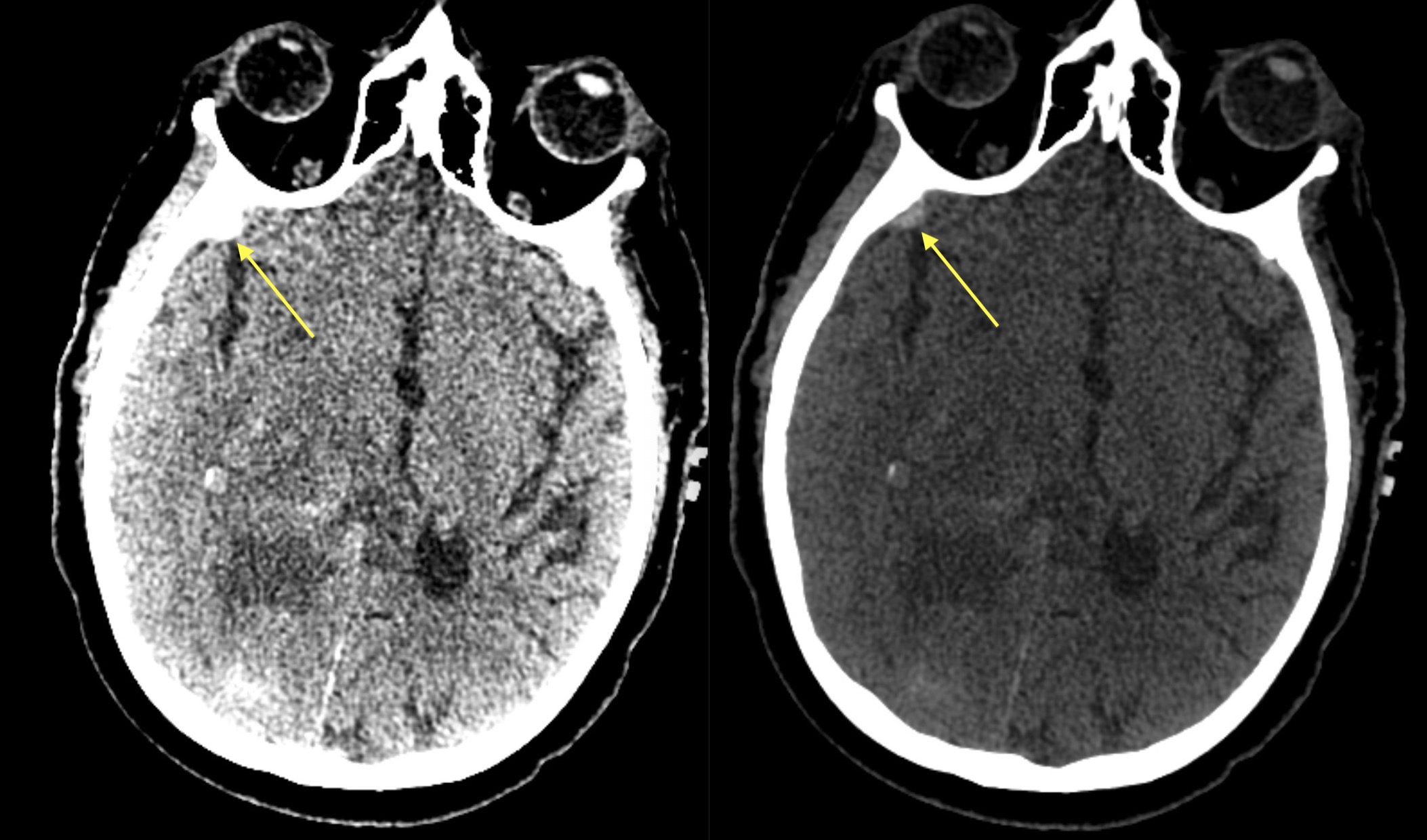
Window for success: Often times it is important to use a special window/level to detect extra axial blood products (called a subdural/epidural window). There is not on standard value set for this (as the thickness and density of the skull will impact the values that are needed) however general values that can be used as a starting point are listed below:
- Level: 50-100 HU
- Window: 100-250 HU
This may take some manual adjustment however the base principle is that the window/level should help make it easy to differentiate subdural blood from adjacent bone.
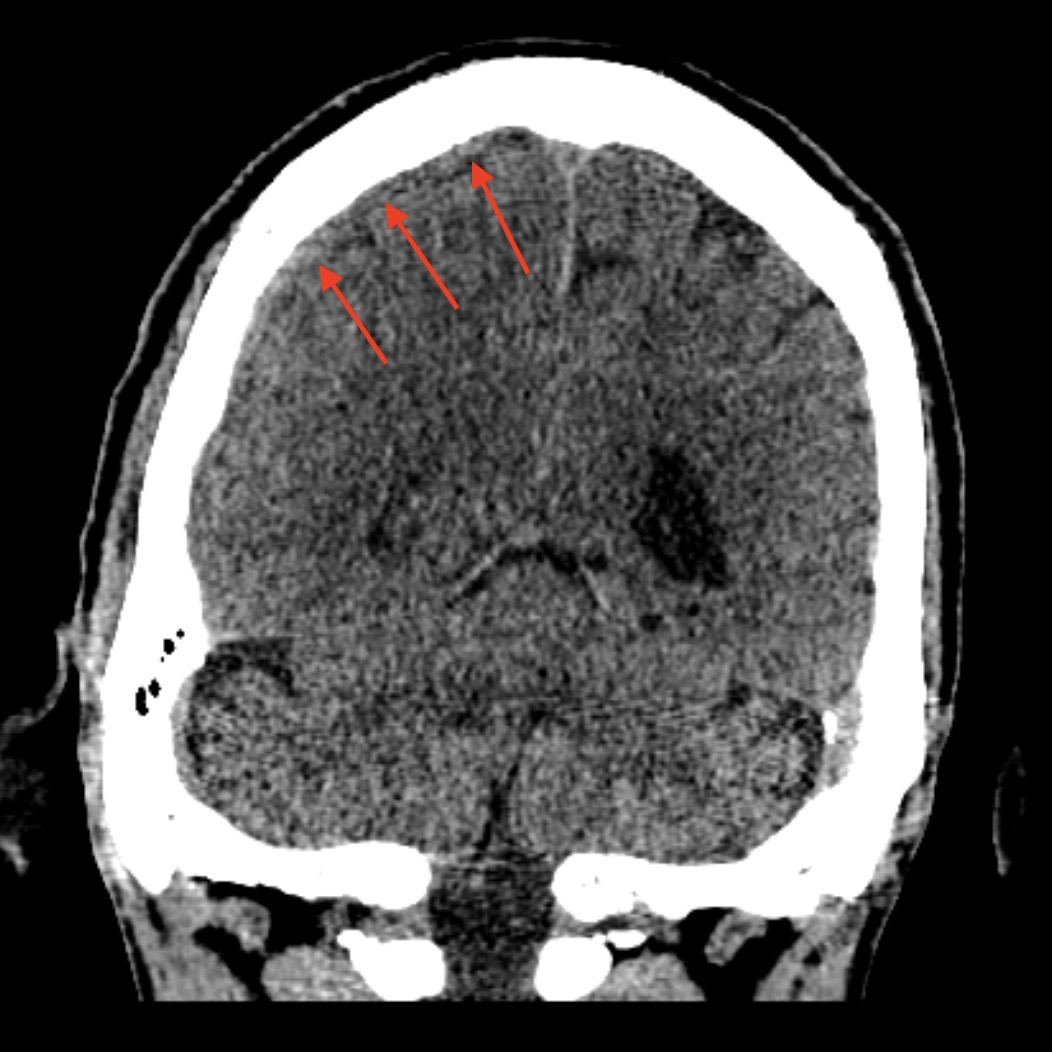
Use reformats (especially coronals): given the shape and location of certain subdural hematomas, many may not be too apparent on standard axial images. Blood products at the vertext, in the middle cranial fossa, or hematomas that are largest in the cranio-caudal dimension all may be more apparent on coronal imaging.
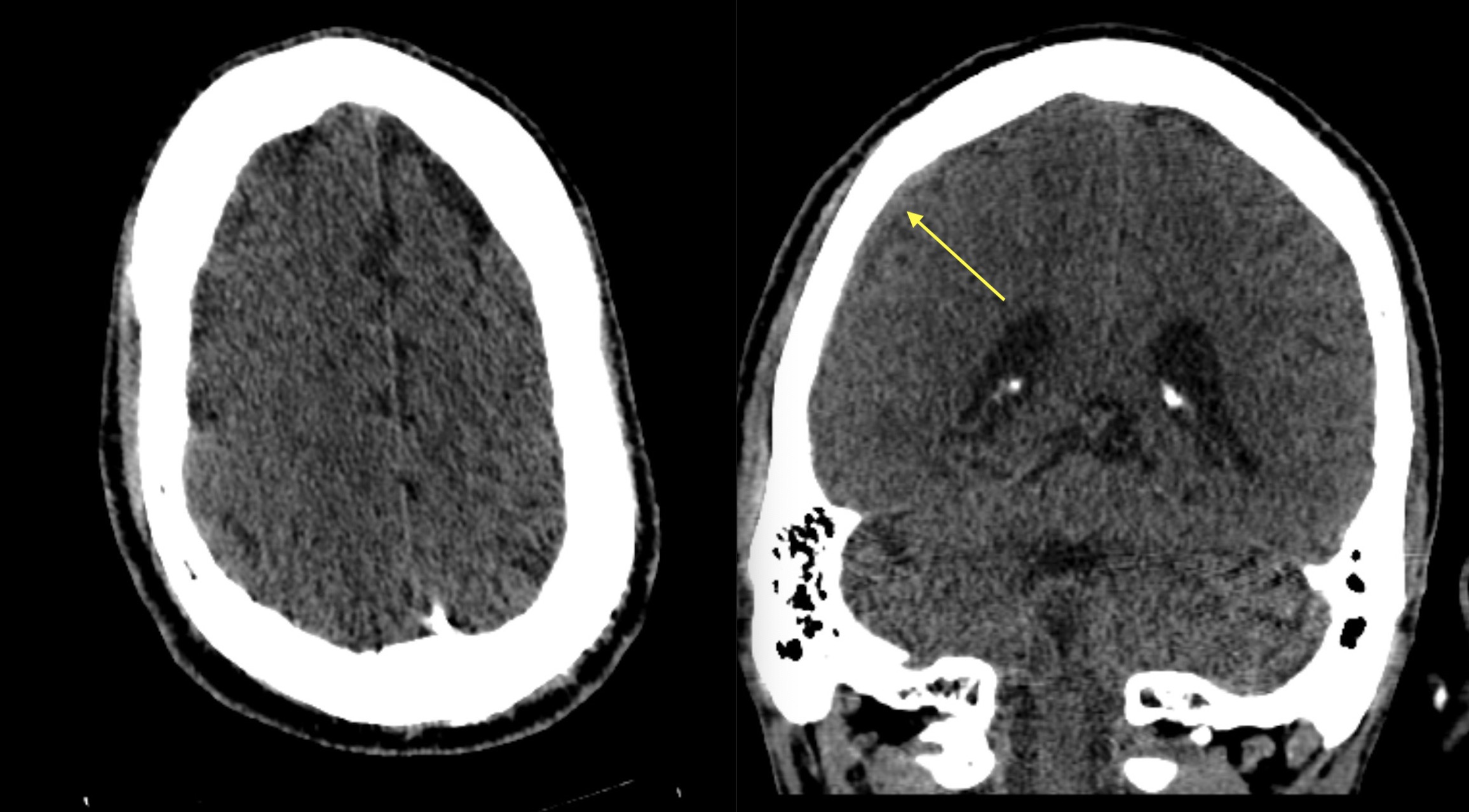
Always make sure to look for extra-axial blood products on both axial and coronal images. In certain cases, sagittal imaging may also be useful to evaluate for a subdural hematoma.
Using Density to Inform Acuity:
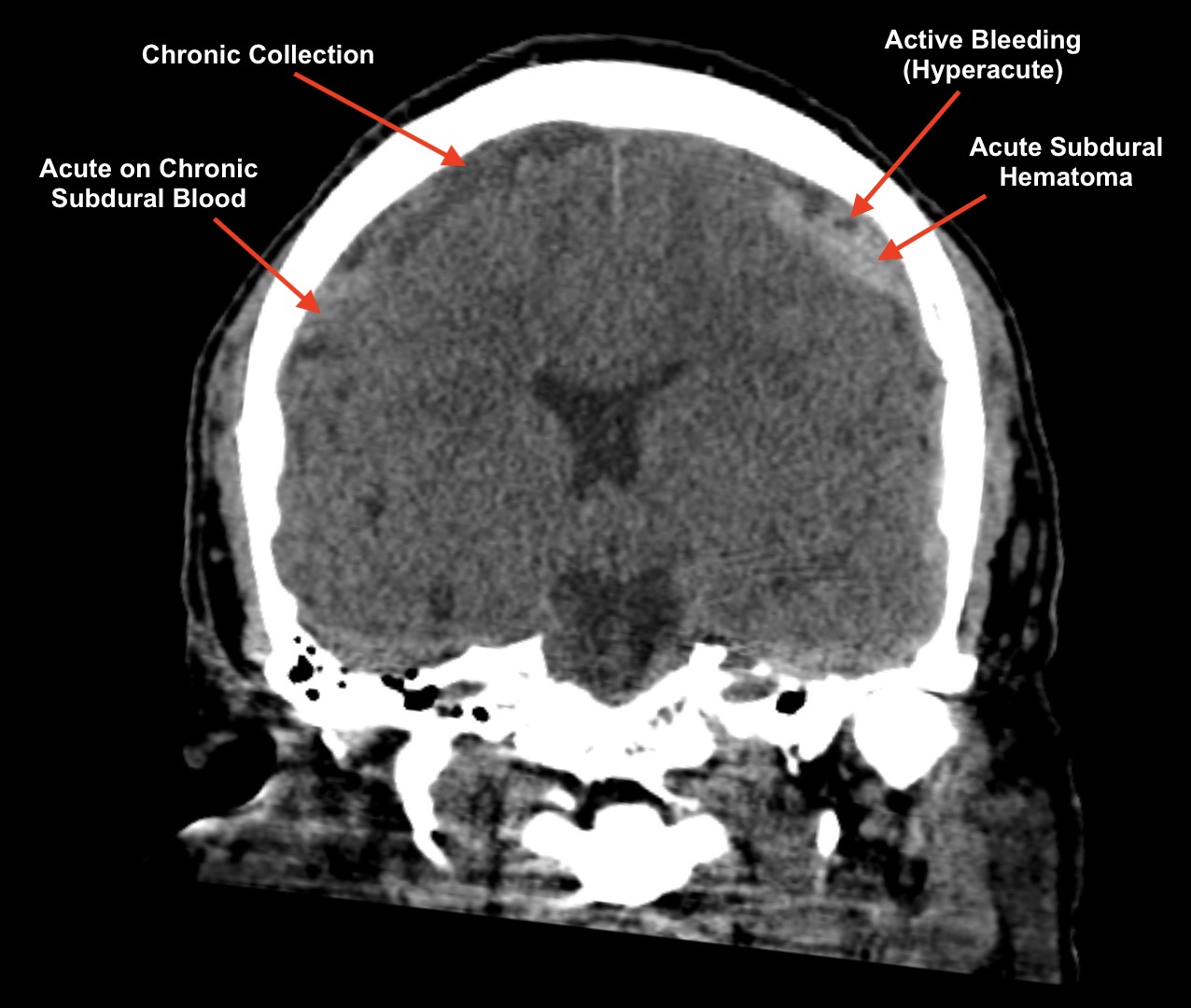
In addition to detecting subdural hematomas, often it is worth understanding the relationship between the age and density of thee blood products. Here is a helpful method of how to think about things;
- Hyper-acute blood is actually very low density (similar to CSF). Typically subdural hematomas with active bleeding will have areas of high density mixed with very low density.
- Acute blood is typically hyper-dense relative to brain parenchyma, although sometimes it can be isodense.
- Subacute blood is typically isodense to the brain parenchyma.
- Chronic blood products are hypo-intense
- Hygromas are chronic fluid subdural collections. These are very low density like CSF. Notably in some instances these may appear identical to chronic blood products. Additionally after IV contrast administration these hygromas will demonstrate contrast staining (making them sometimes look like acute subdurals).
Detecting a subdural hematoma is the first step, but then make sure to look for clues regarding the acuity. When in doubt hedge on the side of acute blood (especially with the right clinical history and in the absence of priors).
WHAT HAPPENS NEXT AFTER THE DIAGNOSIS IS MADE?
Once intracranial hemorrhage is detected on imaging (such as a subdural hematoma), the patient’s trajectory is changed. In most cases a neurosurgical service is consulted (in case there is a need for surgical decompression), the patient is observed more closely (to ensure they do not have a sharp decline in neurological status), a follow up CT scan is ordered (often in 6 hours to evaluate for stability of the bleed), and in many cases a patient’s anticoagulation management is altered (in order to not worsen the bleed).
In brief if there is an isolated subdural hematoma that is missed (and there are no other findings) this can have a significant impact on the patient’s management, so it is important to detect these accurately on call!
CASE ARCHIVE
Use the following login information to access the case archives: USERNAME: user, PASSWORD: password.
Click here to open up a case archive of subdural hematoma cases seen on non-contrast head CT scans.
Page Updated: 11.01.22