Page Contents
OVERVIEW
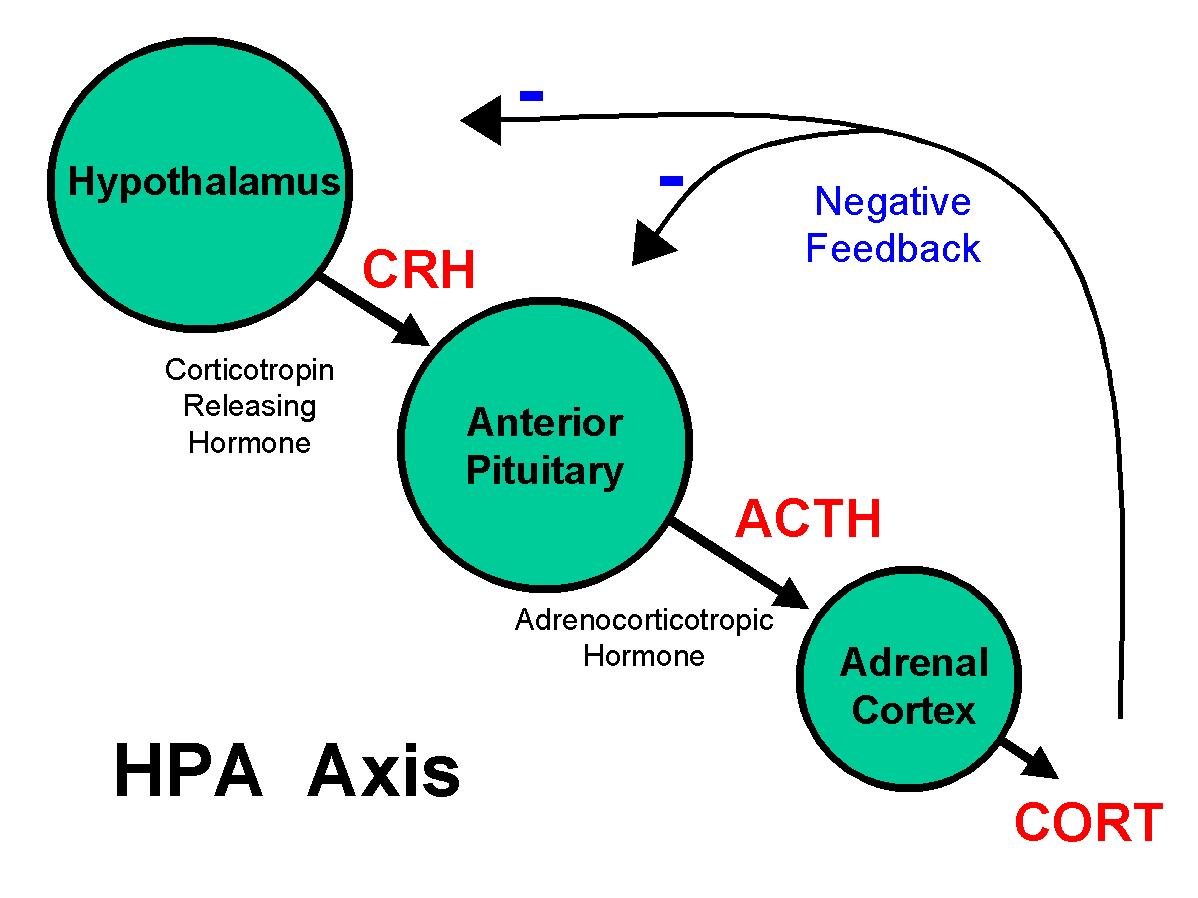
This page focuses on the hormonal pathways that control the production of cortisol (glucocorticoid). Cortisol is an important hormone in mediating the “stress response” and the following signaling pathway is a simplification of how its production is regulated.
Stressor => CRH (hypothalamus) => ACTH (pituitary) => Cortisol (adrenal) => response
HYPOTHALAMUS
The hypothalamus starts off this hormonal pathway by the release of corticotropin releasing hormone (CRH) which in turn acts upon the anterior pituitary to further propagate this signaling pathway (by causing the release of ACTH).
Factors that increase CRH secretion include the following:
- Stress
Factors that decrease CRH secretion include the following:
- Cortisol (negative feedback)
ANTERIOR PITUITARY
The anterior pituitary continues this signaling pathway by releasing adrenocorticotropic hormone (ACTH). ACTH is prepared (cleaved) from a larger pro-opiomelanocortin (POMC) precursor molecule. Once ACTH is in its final form, it can be transported to the adrenals where it can activate downstream signaling pathways. ACTH has the following activity on the adrenal:
- Induce cortisol release (renal cortex): perhaps what most commonly comes to mind, ACTH increases de novo synthesis and secretion of the cortisol (a glucocorticoid). Cortisol mediates the stress response physiologically (more on this later).
- Induce aldosterone release (renal cortex): a mineralocorticoid, aldosterone increases as circulating levels of ACTH increase. It increases solute and water retention in the kidneys which will increase blood pressure and lower urine output.
- Maintain adrenal trophic response: sustained levels of ACTH are important for maintained the adrenal (too much => hypertrophy, too little => hypotrophy).
Factors that increase ACTH secretion include the following:
- CRH: This is the most potent activator of ACTH.
- ADH: While with weaker activity, ADH also will activate ACTH. Furthermore it also inhibit diuresis. (made in the hypothalamus, released by posterior pituitary)
- Oxytocin: this is the “love drug”, very powerful positive feelings associated with its release. This also activates ACTH.
- Epinephrine: This also activates ACTH
Factors that decrease ACTH secretion include the following:
- Cortisol (negative feedback)
ADRENAL GLAND
For the sake of simplicity we will only focus on one hormone from the adrenal gland. As stated before ACTH will induce the release of cortisol by the adrenal gland. Let us keep in mind that cortisol antagonizes ACTH, CRH, and ADH (negative feedback).
Factors that increase cortisol secretion include the following:
- ACTH
Factors that decrease cortisol secretion include the following:
- Loss of ACTH
WHAT DOES CORTISOL ACTUALLY DO?
Up until now we have talked about how cortisol “mediates the stress response” which is a very vague phrase. Glucocorticoids like cortisol act upon nuclear hormone receptors (very much like I3) that act as transcription factors to regulate gene expression. The implications of this can include:
1.) Increased blood sugar: during a stressful experience, it would make sense physiologically to maintain/increase the amount of sugar available in the blood.
- Increase gluconeogenesis: elevated gene expression of important enzymes.
- Promote net protein breakdown: use convert amino acids to glucose.
- Augment epinephrine-mediated lipolysis
2.) Increase vascular constriction:
- Increases α1-receptors on arterioles (which increases sensitivity to catecholamines)
- Increase pressor responses to norepinephrine, angiotensin II
- *Stimulate synthesis of epinephrine in adrenal medulla
- Inhibit tissue uptake of catecholamines: this will leave more free to act on smooth muscles that control vasculature.
- Inhibit synthesis of nitric oxide (a potent vasodilator)
3.) Suppress the immune system through various mechanisms:
- Inhibit production of leukotrienes and prostaglandins
- Inhibit WBC adhesion
- Block histamine releasee from mast cells
- Reduce number of eosinophils
- Block IL-2 production
4.) Affect the CNS: it can affect ones appetite (by increasing it) and overall neural function.
5.) Decreases bone formation (decreases osteoblast activity)
Page Updated: 02.20.2016