Page Contents
- 1 WHAT IS IT?
- 2 WHY IS IT A PROBLEM?
- 3 WHAT MAKES US SUSPECT IT?
- 4 HOW DO WE CONFIRM A DIAGNOSIS?
- 5 HOW DO WE RULE OTHER DIAGNOSES OUT?
- 6 HOW DO WE TREAT IT?
- 7 HOW WELL DO THE PATIENTS DO?
- 8 WAS THERE A WAY TO PREVENT IT?
- 9 WHAT ELSE ARE WE WORRIED ABOUT?
- 10 OTHER HY FACTS?
- 11 ARCHIVE OF STANDARDIZED EXAM QUESTIONS
- 12 FURTHER READING
WHAT IS IT?
Whipple disease is an infectious condition of the small intenstine caused by Tropheryma whipplei (a gram positive bacillus).
WHY IS IT A PROBLEM?
Macrophages within the small bowel lamina propria take up these Tropheryma whipplei bacterium which in turn impairs the ability of the enterocytes to transfer chylomicrons from the enterocytes to the lymphatics. This leads to fat malabsorption and steatorrhea.
Other sites of involvement can include the joints, heart valves, and CNS which lead to impaired functor of these respective structures/systems.
WHAT MAKES US SUSPECT IT?
Risk factors: older caucasian males, exposure to sewage/soil (risk factor for infection).
Common clinical presentation can include the following:
- Weight loss
- Diarrhea (steatorrhea)
- Abdominal pain
- Arthritis
- Fever
- Adenopathy
Neurological symptoms are common with (encephalitis specifically):
- Headache
- Memory impairment
- Dementia
- Cerebellar ataxia
Cardiac symptoms are also sometimes present (in the form of endocarditis)
HOW DO WE CONFIRM A DIAGNOSIS?
*Endoscopic biopsy is most commonly performed for diagnosis.
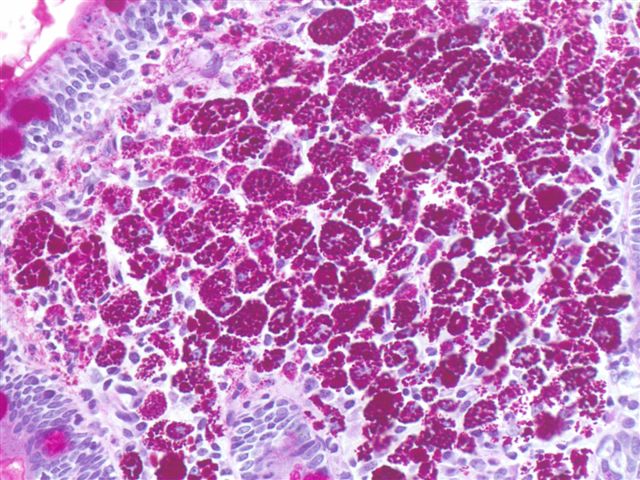
Histology: foamy macrophages can be seen in the intestinal lamina propria.
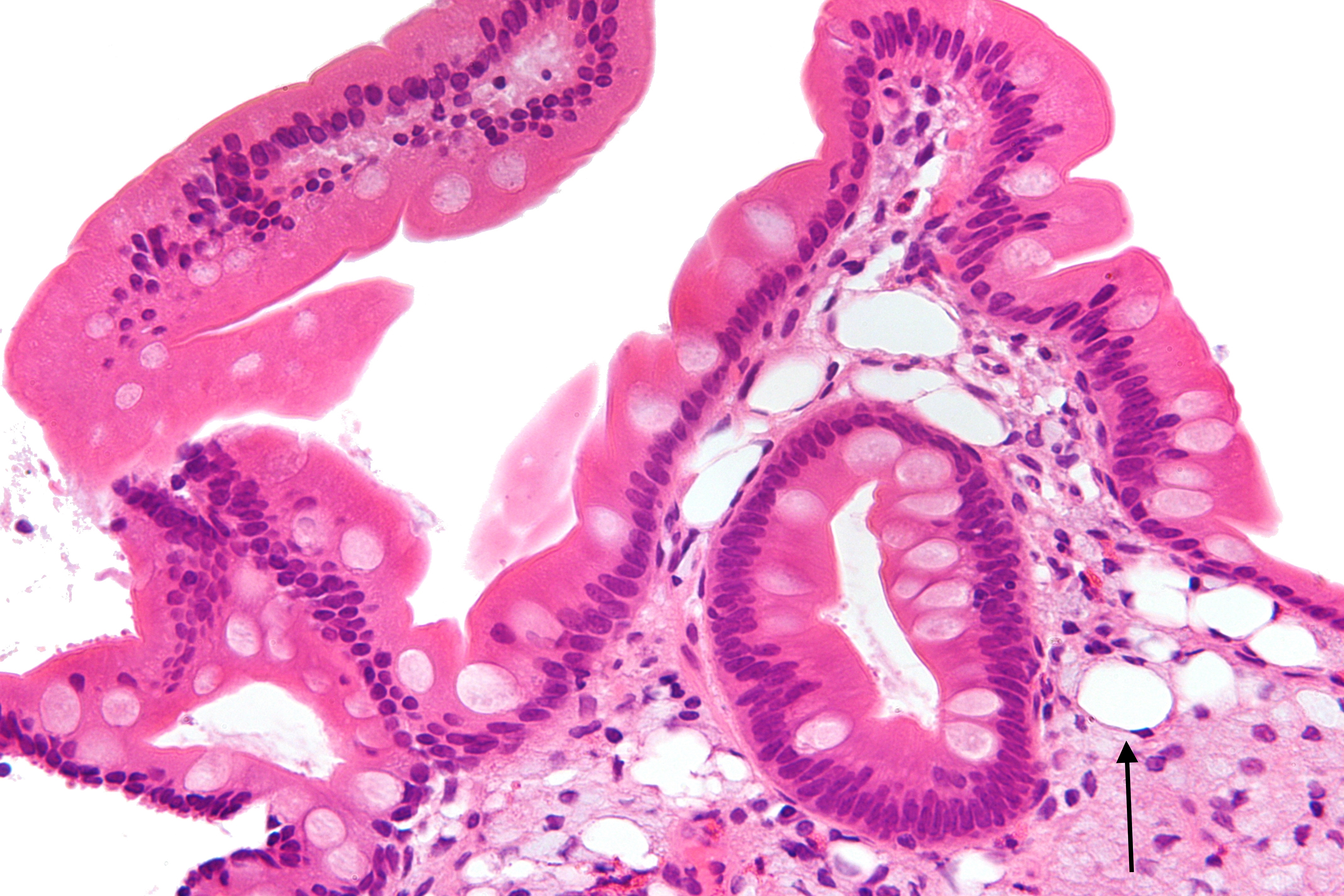
A PAS (periodic acid–Schiff) stain is used to diagnose Whipple disease. Partially digested bacteria inside the macrophages are PAS positive.
PCR can be conducted on tissue sample in order to assess of the presence of T. whipplei. This will provide a definite diagnosis of Whipple disease that is active in the tissue (some individuals can be inactive carriers) so PCR on stool/saliva is not definitively diagnostic.
HOW DO WE RULE OTHER DIAGNOSES OUT?
The intestinal biopsy (especially for PAS and PCR) can help rule out the possibility of the other conditions that present similarly (such as celiac disease).
HOW DO WE TREAT IT?
Long term antibiotics are used however no one regiment is the standard of care:
- Trimethoprim-sulfamethoxazole is a common regiment
- Doxycycline plus hydroxychloroquine is recommended by some
HOW WELL DO THE PATIENTS DO?
Without the usage of antibiotics this disease is fatal. Even with the usage of antibiotics the disease course is persistent and relapse is common.
WAS THERE A WAY TO PREVENT IT?
Avoiding the initial source of infection will prevent this condition (transmission is believed to be oral-fecal).
WHAT ELSE ARE WE WORRIED ABOUT?
Immune reconstitution syndrome is a risk of antibiotic usage. As the immune system recovers from infection, it may “over-respond” to the T. whipplei infection, leading to a worsening of symptoms.
OTHER HY FACTS?
Most infected individuals are able to effectively clear the infection without symptoms. It is only a small subset that have persistent replications of the pathogens in their macrophages causing Whipple disease.
ARCHIVE OF STANDARDIZED EXAM QUESTIONS
This archive compiles standardized exam questions that relate to this topic.
FURTHER READING
Page Updated: 02.20.2016