Page Contents
- 1 WHAT IS IT?
- 2 WHY IS IT A PROBLEM?
- 3 WHAT MAKES US SUSPECT IT?
- 4 HOW DO WE CONFIRM A DIAGNOSIS?
- 5 HOW DO WE RULE OTHER DIAGNOSES OUT?
- 6 HOW DO WE TREAT IT?
- 7 HOW WELL DO THE PATIENTS DO?
- 8 WAS THERE A WAY TO PREVENT IT?
- 9 WHAT ELSE ARE WE WORRIED ABOUT?
- 10 OTHER HY FACTS?
- 11 ARCHIVE OF STANDARDIZED EXAM QUESTIONS
- 12 FURTHER READING
WHAT IS IT?
Crohn disease is an autoimmune inflammatory bowel condition (inflammatory bowel disease/IBD) that can involve any portion of the GI tract (usually terminal ileum and colon, but can be anywhere from the mouth to the anus). Exact cause unknown , however multiple factors seem to contribute to this condition.
WHY IS IT A PROBLEM?
Chronic inflammation in the bowels will cause a host of different complications (see more in the “what else are we worried about?” section) that can include damage to the bowel walls as well as a diminished ability to absorb nutrients (which both can lead to diarrhea).
WHAT MAKES US SUSPECT IT?
Risk factors: HLA-B27, family history,
Clinical symptoms:
- Abdominal pain in the right lower quadrant
- Diarrhea that could or could not be bloody. Sustained diarrhea for greater then 4 weeks is a possible sign of Crohn disease.
- Nausea
- Vomiting
- Constipation
Migratory polyarthritis can be present in patients. Arthritis of multiple joints that moves around the body.
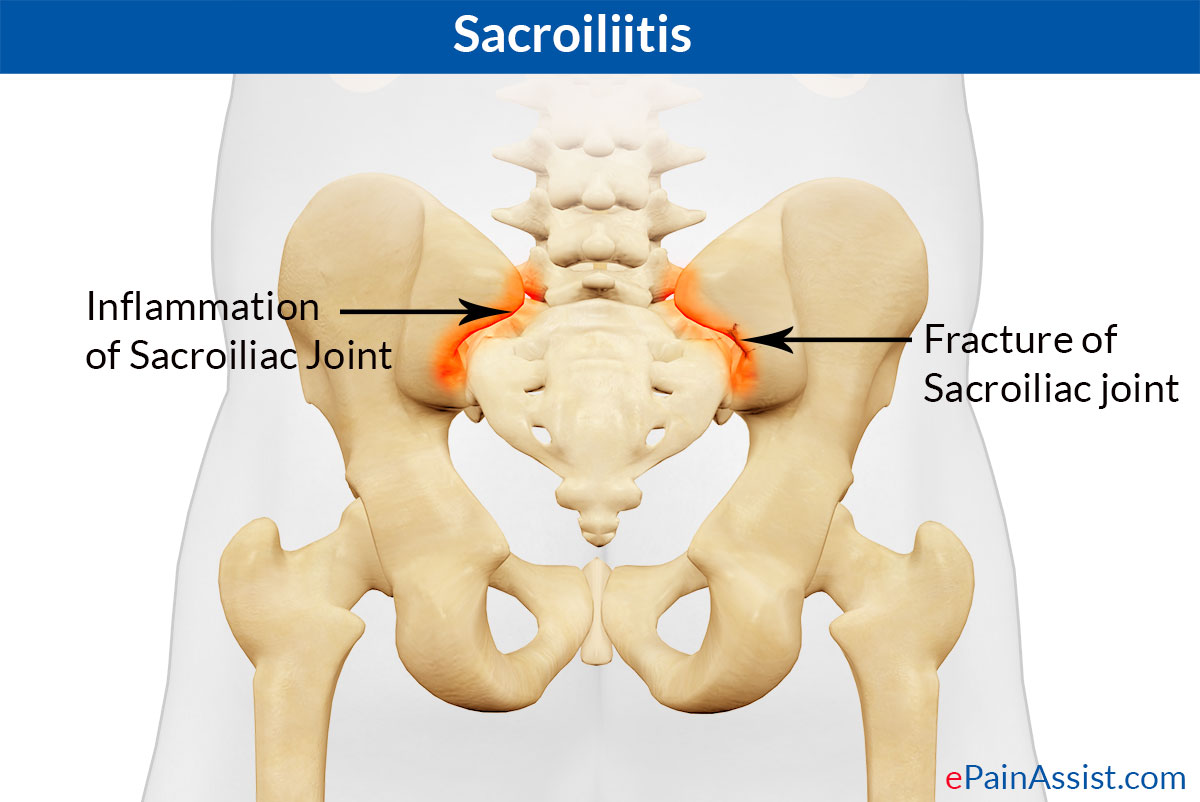
Sacroiliitis: this is the inflammation of one/both of the sacroiliac joints. This can present with pain in the buttocks/lower back and can extend down the legs.
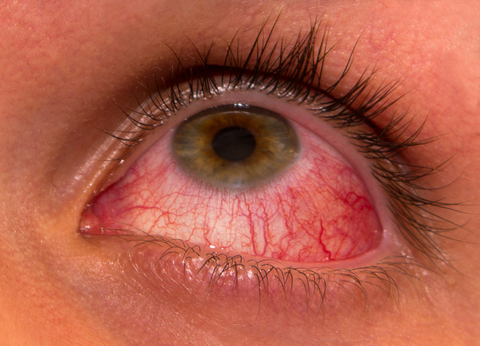
Uveitis: a form of eye inflammation. It affects the middle layer of tissue in the eye wall (uvea).
Possible dermatological fidings:
Erythema nodosum are these tender bumps (nodules) that are under the skin (painful inflammatory lesions of subcutaneous fat).

Pyoderma gangrenosum is a ulcerative cutaneous condition (characterized by the presence of necrotic tissue) that can be seen in Crohn disease.

Aphthous ulcers are the formal name for canker sores that can sometimes be seen in patients with Crohn disease (anywhere in the GI tract).

HOW DO WE CONFIRM A DIAGNOSIS?
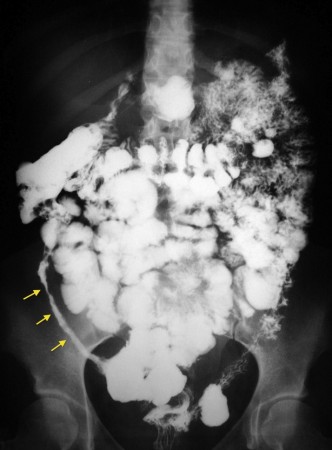
Barium swallow x-ray: a classic “string sign” can be seen with this type of imaging due to bowel wall thickening.
Gross pathology (endoscopy) of Crohn disease can have some of the following findings:
- Cobblestone mucosa
- Creeping fat
- Bowel wall thickening
- Linear ulcers (that are transmural and discontinuous)
- Fissures

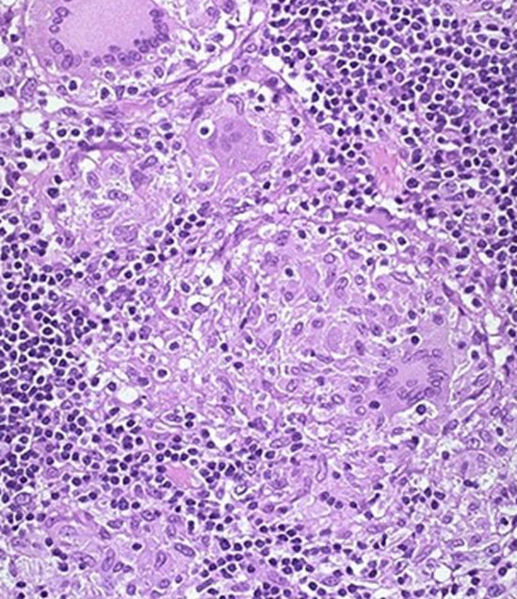
Histology can reveal noncaseating granulomas and lymphoid aggregates (that are Th1 mediated) and transmural inflammation.
HOW DO WE RULE OTHER DIAGNOSES OUT?
*Distinguishing between ulcerative colitis and Crohn disease is important when putting together a differential diagnosis!
Symptoms of diarrhea: ulcerative colitis ususlly causes bloody diarrhea while Crohn disease only will present with bloody diarrhea part of the time.
Distribution of inflammation: there are clear differences in the patter of inflammation seen in Crohn disease vs. ulcerative colitis.
- Crohn disease involves any portion of the GI tract, the lesions are not continuous (skip lesions) and the rectum is spared. Transmural inflammation present.
- Ulcerative colitis refers to inflammation that is in the terminal GI tract (colon), the lesions are continuous, and it always involves the rectum. Mucosal/submucosal inflammation only.
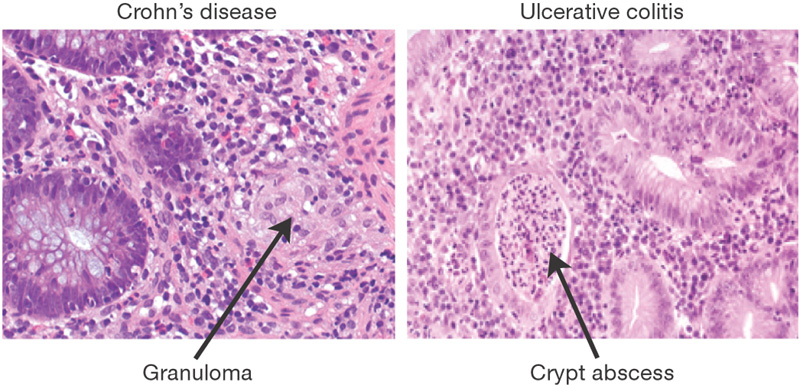
Histological analysis can be very useful in informing the diagnosis between Crohn disease and ulcerative colitis. Crohn disease is characterized by the presence of non-caseating granulomas, while ulcerative colitis will possess crypt abscesses.
HOW DO WE TREAT IT?
Corticosteroids, azathioprine, antibiotics (e.g., ciprofloxacin, metronidazole), infliximab, adalimumab.
Corticosteroids can be used to antagonize mechanism of inflammation.
Tumor necrosis factor inhibitors/anti-TNF (infliximab, adalimumab): these medications are antibodies that bind and antagonize TNF-alpha
Natalizumab: is an antibody agains α4-integrin (protein used in WBC adhesion)
Sulfasalazine: this is a combination of sulfapyridine (antibacterial) and 5-aminosalicylic acid (anti-inflammatory) that is selectively activated by bacteria in the colon.
Azathioprine: this is an antimetabolite precursor of 6-mercaptopurine. This medication inhibits lymphocyte proliferation by blocking nucleotide synthesis. *LIMITED AND INCONSISTENT EVIDENCE FOR INDUCING REMISSION AS A MONOTHERAPY
Antibiotics (e.g., ciprofloxacin, metronidazole) should be used in patients with infection/at risk of infection due to fissure/abscess formation.
Cholestyramine: is a bile acid binding resin that can be used in patients who have diarrhea caused by the presence of residual bile salts in the bowel.
Surgery while not curative can help address some symptoms by the resection of symptomatic lesions/bowel pathology. A risk of repeat surgical resection is the development of short bowel syndrome (a decrease in the length of the bowel to the point that nutrients are not able to be effectively absorbed).
HOW WELL DO THE PATIENTS DO?
This condition often presents with serious complications (explained above in the “what else are we worried about?” section) and is not curable. It has a chronic/relapsing course.
WAS THERE A WAY TO PREVENT IT?
There is no clear means of preventing the development of Crohn disease.
WHAT ELSE ARE WE WORRIED ABOUT?
Obstruction can occur as a result of stricture formation. This is a serious complication that often requires surgical intervention.
Fistula formation: because Crohn disease exhibits transmural inflammation of the bowel wall, the formation of fistulas.
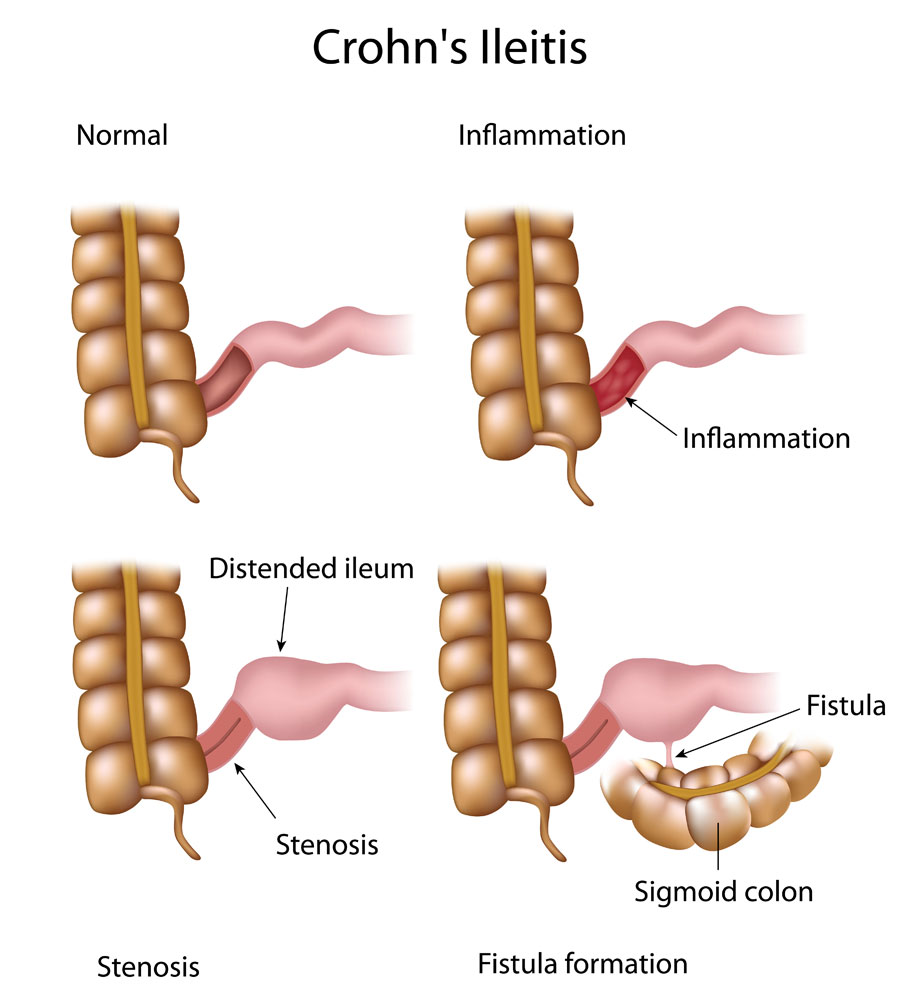
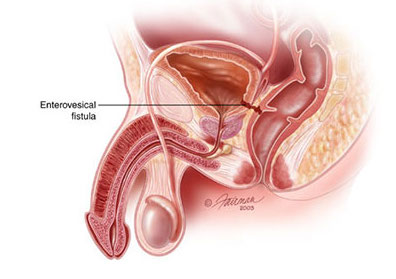
Enterovesical fistulae refers to a fistula the occurs between the bowel and the bladder. This can be a complication of Crohn disease that will lead to recurrent polymicrobial UTIs).
Abscess formation can occur due to infection of damaged tissues.
Absorption deficiency:
- Vitamin B12 deficiency: patients who are missing the terminal ileum (either to damage/surgery from Crohn disease) can have issues absorbing vitamin B12 (because this is where vitamin B12 is absorbed).
- Fat soluble vitamin (A, D, E, and K): a relative lack of bile salts can lead to impaired absorption of these fat soluble vitamins.
- Folate deficiency: can also be caused by Crohn disease.
Ankylosing spondylitis: a form of spinal arthritis that is characterized by the fusion of these joints together.
Kidney stones (calcium): can form in patients with Crohn disease
Gall stones formation is assocaited with Crohn disease
Colon cancer: risk can be elevated in patients with Crohn disease.
OTHER HY FACTS?
Bimodal distribution increased presentation seen in age groups of 15-30 and 60-80 years of age.
ARCHIVE OF STANDARDIZED EXAM QUESTIONS
This archive compiles standardized exam questions that relate to this topic.
FURTHER READING
Page Updated: 02.17.2016