Page Contents
OVERVIEW
This page is dedicated to organizing various examples of standardized exam questions whose answer is heparin induced thrombocytopenia (HIT). While this may seem a odd practice, it is useful to see multiple examples of how HIT will be characterized on standardized exams (namely the boards and the shelf exams). This page is not meant to be used as a traditional question bank (as all of the answers will be the same), however seeing the classic “test” characterization for a disease is quite valuable.
KEY CHARACTERISTICS OF THIS CONDITION (ON EXAMS)
When it comes to standardized exams, each topic has its own “code” marked by key buzzwords, lab findings, clues, etc. If you are well versed in this code you will be able to more quickly identify the condition that is being discussed, and get the right answer on the exam you are taking. Below is the “code” for HIT.
Chief Complaints:
- Presence of bruises/ecchymoses or unexplained bleeding
Patient History:
- Recent heparin administration: this is a necessary component of the medical history (can’t be heparin induced if there is no heparin!). Often times heparin is administer 5-10 days before onset of symptoms.
- Signs of new/worsening thrombosis AFTER heparin administration: paradoxically HIT can cause new thrombosis (or cause a worsening of a current thrombosis) in patients after it occurs.
Clinical workup
- Low platelets (thrombocytopenia) will be detected on a CBC.
- Coagulation studies will reveal
- Elevated bleeding time, due to low platelets.
- Normal PT time, this coagulation pathway is not affected by this condition
- Normal PTT time, this coagulation pathway is not affected by this condition
QUESTION EXAMPLES
Question # 1
A few days after undergoing a coronary artery bypass surgery, a hospitalized 50 year old man begins to experience sever pain in his left toe. He initially presented to the hospital 9 days ago for the evaluation of exertion chest pain, and received heparin for 3 days. The operation was uncomplicated and the patient’s postoperative course was unremarkable. Vital signs are within normal limits. A physical exam reveals a tender and cyanotic left great toe. There are new ecchymoses present over the trunk and lower extremities. The surgical incision is clean/dry/intact. Labs are conducted and shown below:
- Hematocrit: 38%
- Leukocyte count: 11,900/mm3
- Platelet count: 7,900/mm3 ***
- PT: 12 seconds (INR = 1) ***
- PPT: 17 seconds ***
What is a possible diagnosis?
Explanation # 1
Recent heparin usage + low platelets + normal PT/PPT times = HIT
Question # 2
A 60-year-old woman comes to the clinic because her right leg is swollen and tender. Her past medical history is remarkable for ovarian cancer and she is currently undergoing chemotherapy. A duplex Venus ultrasound study of her right lower leg shows a thrombosis in the right popliteal vein. The patient is sent home with subcutaneous enoxaparin. One week later the patient comes back to the clinic for a follow up appointment.
- Hematocrit: 44% (45% last week)
- Leukocytes: 6,200/mm³ (6,100/mm³ last week)
- Platelets: 65,000/mm³ (230,000/mm³ last week) ***
- INR: 1.0 (0.9 last week) ***
What is the likely cause of this patients thrombocytopenia?
Explanation # 2
Recent drop in platelets after heparin usage (enoxaparin) + normal INR = HIT
Question # 3
A 45 year old male is hospitalized with unstable angina. He is treated with various medications, including heparin for anticoagulation. On the 6th day of his hospital mission, he develops significant left foot pain and his left toe becomes pale. His labs are collected and his platelet count is found to be 50,000/mm³. What diagnosis needs to be considered in this patient?
Explanation # 3
Recent heparin usage + low platelets + signs of new thrombosis in left foot = HIT
Question # 4
A 25 year old female develops deep vein thrombosis during the 5th month of her pregnancy. IV heparin is started for anticoagulation therapy. A week later her platelet count is found to be 45,000/mm³. What is the most likely cause of this patient’s lab abnormality?
Explanation # 4
Recent heparin usage + low platelets = HIT
Question # 5
A 40 yar old female comes to the clinic because she has been feeling pain in her right leg for the past few days. A physical exam is conducted and shows that she has a deep vein thrombosis in her right lower leg. Labs are collected and the patient is noted to have a platelet count of 220,000/mm³ and her INR is 1.0. She is started on heparin therapy. A well later the patient’s physical exam is unremarkable, however her platelet count is now 100,000/mm³. What is the likely cause of this patient’s drop in platelets?
Explanation # 5
Recent heparin usage + low platelets = HIT
Question # 6
A 75 year old female is admitted to the hospital because she recently has developed a large pulmonary embolism. Her platelet count is currently 170,000/mm³. Appropriate treatment is started promptly. A week later her routine labs reveal a platelet count of 50,000/mm³. What is the likely cause of this patient’s drop in platelets?
Explanation # 6
Recent heparin usage (appropriate treatment for pulmonary embolism) + low platelets = HIT
Question # 7
A 60 year old woman comes to ED because she has been experiencing left foot swelling and tenderness for the past few days. Her past medical history is notable for end stage renal disease and she is hemodialysis dependent. A lower extremity duplex study reveals the presence of a deep vein thrombosis in her left foot that is thought to be responsible for her symptoms. She is started on an IV heparin infusion and is admitted to the hospital for further management. On the 5th day of her admission, her left leg becomes even more swollen and painful. A repeat ultrasound study shows further extension of the thrombus in her left leg. Labs are collected and shown below:
- Hemoglobin: 13.5 g/dL
- Platelets: 40,000/mm³ ***
- WBC: 7,000/mm³
- PTT: WNL
What is the likely cause of the patient’s worsening condition?
Explanation # 7
Recent heparin usage + low platelets + signs of worsening thrombosis = HIT
TESTABLE FACTS ABOUT THIS TOPIC (BEYOND ITS IDENTIFICATION)
Many questions on standardized exams go beyond simply recognizing the underlying topic. Often there are specific testable facts regarding some aspect of the topic’s pathophysiology/management/clinical implications that are commonly asked. Some of these are listed below:
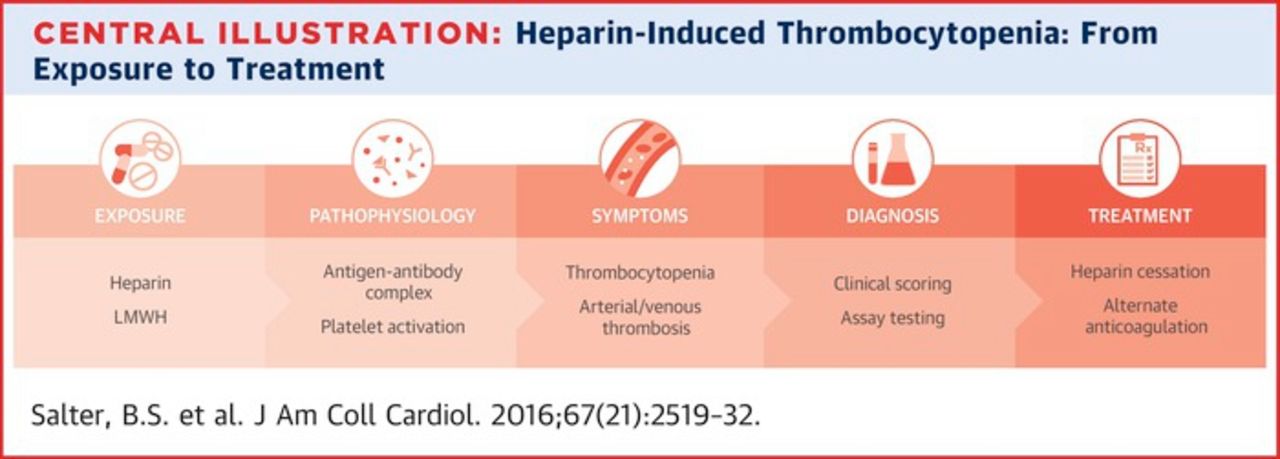
Cause
- Recent heparin usage causing autoantibodies against platelets.
- IgG antibodies against heparin-bound platelet factor 4: (anti-platelet antibodies) this antibody-antigen complex activates platelets and causes thrombosis/low platelets.
Treatment
- Discontinue all heparin treatments: this should be done immediately after HIT is diagnosed.
- Direct thrombin inhibitors (argatroban, hirudin, lepirudin) should be used for further anticoagulation: patients with HIT will still need anticoagulation. These drugs do not require antithrombin-III for their desired effect, and are the drugs of choice in HIT.
Page Updated: 01.22.2017