Page Contents
OVERVIEW
This page is dedicated to organizing various examples of standardized exam questions whose answer is celiac disease. While this may seem a odd practice, it is useful to see multiple examples of how celiac disease will be characterized on standardized exams (namely the boards and the shelf exams). This page is not meant to be used as a tradition question bank (as all of the answers will be the same), however seeing the classic “test” characterization for a disease is quite valuable.
KEY CHARACTERISTICS OF THIS CONDITION (ON EXAMS)
When it comes to standardized exams, each topic has its own “code” marked by key buzzwords, lab findings, clues, etc. If you are well versed in this code you will be able to more quickly identify the condition that is being discussed, and get the right answer on the exam you are taking. Below is the “code” for celiac disease.
Chief Complaints:
- Diarrhea is a very common complaint (often greasy and malodorous)
- Itchy skin rash usually found on elbows/knees.
Patient History:
- Presence of gluten in diet is not necessarily always stated, however patients should have this exposure (which might be implied by the passage).
Clinical Workup:
- Dermatitis herpetiformis: this skin finding is often present in these patients (erythematous prussic papules, vesicles, and bullae). Usually found on elbows/knees.
- Iron deficiency (and associated anemia) can be found in these patients (due to GI issues of absorbing iron in setting of damage to intensities where it is absorbed)
- D-xylose test (poor absorption of D-xylose): this is a monosaccharide that only requires an intact mucosa to be absorbed. Less will be absorbed in patient’s with celiac disease.
- Endomysial IgA antibody can be detected on serologies (essentially diagnostic).
- Anti-tissue transglutaminase IgA antibodies can be detected on serologies (essentially diagnostic).
- Blunted villi can be seen on a biopsy of the intestine (essentially diagnostic). This can also be called villous atrophy or loss of villi.
QUESTION EXAMPLES
Question # 1
A 15 year old boy is borough tot he clinic because he has been experiencing a skin rash for the past 3 weeks. He first noted these red spots on his arms and legs act were itchy, and since then they have filled with clear fluid. Some of them are crusted over. He explains that he also feels fatigued, and does not have energy to participate in pickup games of basketball after school. His past medical history is notable for type 1 diabetes, and his blood sugars are well controlled with insulin. The patient has lost 10 lbs since his last checkup about 4 months ago. A physical exam reveals conjunctival pallor, and an erythematous vesicular rash that is distributed symmetrically over the extensor surfaces of the elbows and knees. Lab results are collected and shown below:
- Hemoglobin: 9.8 g/dL**
- Mean corpuscular volume: 70 fL**
- Platelets: 235,000/mm³
- Leukocytes: 8,200/mm³
- Ferretin: 9.1 ng/mL**
Fecal occult blood testing is negative. What diagnosis might explain this presentation in this patient?
Explanation # 1
Iron deficiency anemia + vesicular itchy skin rash over elbows/knees (dermatitis herpetiformis) = celiac disease
Question # 2
A 45 year old woman comes to the clinic because she has been experiencing a bloating and diarrhea for “many months”. She explains that she passes many large and foul smelling stools daily. Since her last visit 3 months ago she has lost 30 lb but denies and changes to her diet or appetite. Her past medical history is non-contributory and she is not taking any medications. Her BMI is currently 17 kg/m2. The patient’s vital signs are all within normal limits. A physical exam reveals the presence of a beefy red tongue and mild temporal wasting. The rest of the physical exam is only remarkable for scattered ecchymoses and trace edema over the lower extremities. Labs are collected and the results are shown below.
- Hematocrit: 27%
- Mean corpuscular volume: 65 µm3
- Leukocyte count: 5,200/mm3
- Prothrombin time: 22 sec (INR = 1.5)
- Serum Albumin: 2.5 g/dL
- Endomysial IgA antibody: positive ***
What is the likely diagnosis in this patient?
Explanation # 2
Endomysial IgA antibody = celiac disease
Question # 3
A 16 month old girl is brought to the pediatrician because of a 3-month history of diarrhea. Her parents explain that she has 4-6 loose, non-bloody bowel movements daily. Occasionally the patient also vomits. She as fed with breast milk only until the age of 10 months, and has since had a varied diet that includes: whole milk, bread, fruits, vegetables, and meats. The girl has become less and less interested in eating over the past several weeks. Her past medical history is unremarkable, and she has no history of travel or sick contacts. The patent has lost 3 lbs in the last 3 months. After some lab tests are run, a duodenal biopsy is conducted and shows the following findings:
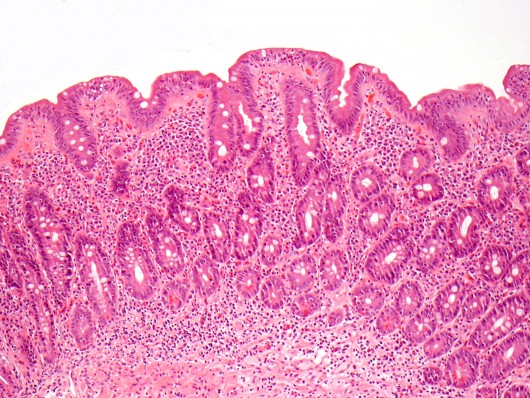
What is the likely diagnosis in this patient?
Explanation # 3
Diarrhea + history of eating gluten products (bread) + blunted villi/villous atrophy (biopsy) = celiac disease
Question # 4
A 12 year old girl is brought to the clinic because she suffers from abdominal discomfort, and has had bloating for several months. This patient also has been passing a large amount of gas daily, and has loose stools. She eats a varied diet. Her past medical history is unremarkable other then a trip to Africa last year with her family for vacation. Her last well child visit with the pediatrician showed no abnormalities. A look at her vitals reveals that she has lost 5 lbs since her last visit, and has not really grown much taller. Her physical exam reveals slight abdominal distention. Serological testing is done that reveals auto-antiboideis that react with tissue transglutaminase. What is the diagnosis in this patient?
Explanation # 4
Diarrhea + auto-antibodies to tissue transglutaminase = celiac disease
Question # 5
A 40 year old male comes to the clinic because he has been suffering from a itchy skin rash over his elbows and knees. He has been using topical creams however the lesions have not gotten better. He also complains of a long history of abodminla discomfort, large volumes of greasy stools, and “farting up a storm”. A physical exam is unremarkable, other than a skin exam that shows a vesicular skin rash that is present in groups with erosions. What is the likely diagnosis in this patient?
Explanation # 5
Diarrhea + vesicular itchy skin rash over elbows/knees (dermatitis herpetiformis) = celiac disease
Question # 6
A 40 year old man has a 5 year history of diarrhea, bloating, and crampy abdominal pain. He complains that his stools are “very greasy and very smelly”. He had similar symptoms as a child, but this resolved spontaneously after his mother started banning processed foods in the house. In addition to his gastro-intenstinal complaints, the patient complains of the following chronic pruitic rash that is seen on his elbow below:

What is the likely diagnosis in this patient?
Explanation # 6
Diarrhea + association of symptoms with processed foods (many of which have gluten) + vesicular itchy skin rash over elbows/knees (dermatitis herpetiformis) = celiac disease
Question # 7
A 30 year male starts to develop loose, malodorous stools that float in the toilet. His proximal intestine is biopsied and shows that he has lost villi (and has a flat mucosa). What is the diagnosis in this patient?
Explanation # 7
Diarrhea + loss of villi on biopsy = celiac disease
Question # 8
A 25 year old woman comes to the clinic because she suffers from a 7 month history of diarrhea, and has lost 20 lbs of weight in the past year. A physical exam shows skin pallor. Lab analysis revel as the presence of increased fat in her stool. Serum serologies reveal the presence of anti-endomysium IgA antibodies, and anti-tussue transglutaminase IgA antibodies are also positive. What is the likely diagnosis in this patient?
Explanation # 8
Diarrhea + anti-endomysium IgA antibodies + anti-tussue transglutaminase IgA antibodies = celiac disease
Question # 9
A 3o year old male comes to the clinic because he has been experiencing fatigue and loose stools for the past 4 months. During this time he has lost about 12 lbs, even though he has a good appetite and has not changed his food intake. His past medically history is notable for a period of childhood diarrhea that self resolved without treatment/intervention. A test of his stool shows no leukocytes, and no pathogens are cultured from the stool sample. A 72 hour test of the stool also shows a large amount of fecal fat. D-xylose absorption testing shows a serum D-xylose concentration below the reference range after the administration of D-xylose. What is the likely cause of this patient’s symptoms?
Explanation # 9
Diarrhea + low absorption of D-xylose after administration = celiac disease
TESTABLE FACTS ABOUT THIS TOPIC (BEYOND ITS IDENTIFICATION)
Many questions on standardized exams go beyond simply recognizing the underlying topic. Often there are specific testable facts regarding some aspect of the topic’s pathophysiology/management/clinical implications that are commonly asked. Some of these are listed below:
Cause:
- Ingestion of gluten/immune meiatred reaction to gluten
Consequences:
- Damage to small intestine mucosa
- Poor absorption in small intestine: patient’s may have issues with absorbing things such as iron (can have iron deficiency anemia)
Diagnosing Celiac Disease:
- Intestinal biopsy (showing blunted villi/intraepithelial lymphocyte infiltration) is the most diagnostic
Treatment:
- Cessation of gluten ingestion
Page Updated: 11.26.2016