Page Contents
WHAT IS IT?
Hodgkin disease/lymphoma (HL) is a neoplasm of the lymphatic system that is characterized by proliferation of large B-cells (more on this later). This disease is usually characterized by the orderly (contiguous) spread of neoplastic cells from lymph node group to lymph node group (usually extra nodular masses will not be present).
Subtypes of the disease include:
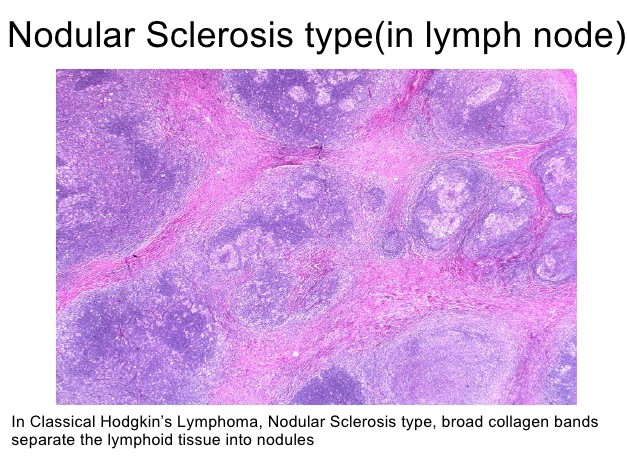
- Nodular sclerosis: most common subtype, associated with fibrosis of the lymph nodes
- Mixed cellularity: second most common is associated with abundant eosinophils
- Lymphocyte-rich: rare
- Lymphocyte depleted: most rare
Cause: the exact precipitating factor is unknown for HL.
WHY IS IT A PROBLEM?
The cells that compose the lymphoma (Reed-Sternberg cells discussed more later) secrete cytokines that cause the B symptoms described below (fever, sweats, chills). Furthermore these cytokines attract reactive white blood cells, and also can lead to fibrosis.
WHAT MAKES US SUSPECT IT?
Risk factors: EBV infection, (male, except for nodular sclerosing which affects females more)
Constitutional (“B”) signs/symptoms: these include
- low grade fever
- night sweats
- weight loss
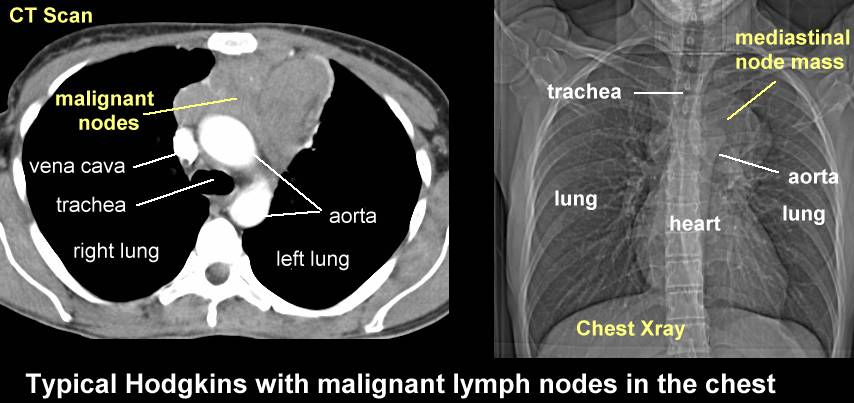
Lymphadenopathy: that will usually not be painful on physical exam. Cervical/subclavicular which can be felt on physical exam, and mediastinal that can be seen on a chest X-ray (perhaps from a previous x-ray the patient has received. Rarely affects the tonsils/adenoids.

Symptoms of mediastinal node swelling: cough, chest pain, dyspnea, swelling in arms/face (due to superior vena cava obstruction by mass)
*Splenomegaly is rare
Skin findings: can include erythema nodosum, and ichthyosis
HOW DO WE CONFIRM A DIAGNOSIS?
Erythrocyte sedimentation rate (ESR) can be elevated (typically in more advanced disease)
Complete blood count findings: depending on the subtype (as well as the possibility of bone marrow involvement) the below findings could be seen in a patient with HL:
- Eosinophilia
- Thrombocytopenia
- Anemia
- Leukocytosis
- Lymphocytopenia
CT scan can be used to assess best lymph node to assess for biopsy:
*DIAGNOSED WITH BIOPSY
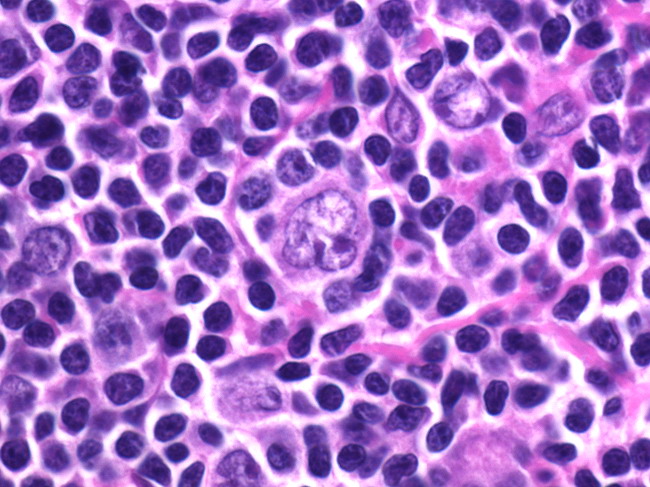
Reed-Sternberg (RS) cells: these are giant cells seen in Hodgkin disease that are binucleate/bilobed eosinophilic nuclei (that are referred to as “owl eyes”) .
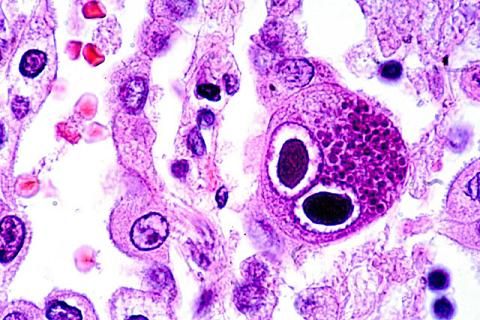
These Reed-Sternberg cells are CD15+ and CD30+ that are of B-cell origin. Non-Hodgkin lymphomas DO NOT HAVE THESE CELLS
*Normocytic anemia can also be present as well (decreased Hg/Hct with normal MCV).
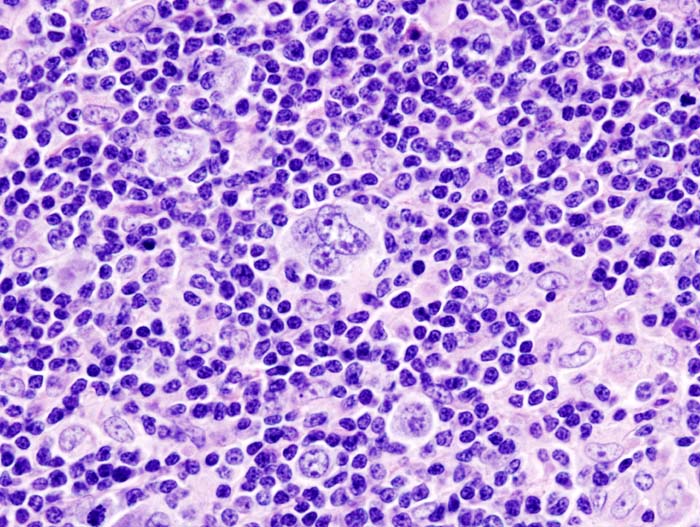
Subtype specific biopsies: characterizing the different types of HL relies heavily upon histology (some examples seen below). The names of the subtypes help describe their respective pathologies.
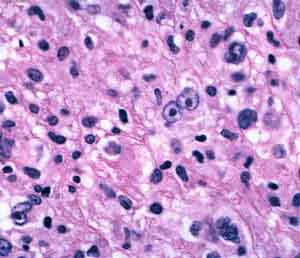
Nodular sclerosis: biopsy reveals prominent collagen deposition/fibrosis. A subtype of the RS cells (called lacunar cells) reside between the divisions of the fibrotic tissues.
Mixed cellularity: There will be prominence of numerous RS cells mixed with different inflammatory cells (lymphocytes, histiocytes, eosinophils, and plasma cells). No surrounding sclerosis observed. *It is possible for this condition to have the mononuclear variant of the RS cells!
Lymphocyte-rich: In these tissues it is difficult to find typical RSCs. Instead lymphohistiocytic variant RSC (popcorn cells) may be seen
Lymphocyte depleted: very few RS cells present or reactive lymphocytes.
HOW DO WE TREAT IT?
*Combination/exclusion of the below treatment options will depend on the specific case of HL
ABVD chemotherapy regimen for (6 to 8 months): this is the standard
- Adriamycin (Doxorubicin): an antibiotic that works by intercalating with DNA (disrupts replication and transcription). It breaks the DNA.
- Bleomycin: this is an anti-tumour antibotic that induces free radical formation that leads to breaks in DNA.
- Vinblastine: this is a microtubule inhibitor used for Hodgkin disease. It binds β-tubulin and inhibits its polymerization into microtubule. These ultimately arrests cells in the M phase of cell division, interfering with microtubule formation.
- Dacarbazine: chemotherapy medication that is an alkylating/methylating drug of DNA (guanine specifically). This inhibits DNA replication.
Radiation: specifically called involved site radiation therapy (ISRT) used to be done regularly but now is more limited in its usage. It can increase risk of cardiac abnormalities and also neoplastic growths in the breast/lung (for mediastinal radiation).
HOW WELL DO THE PATIENTS DO?
*Prognosis is much better than non-Hodgkin lymphoma
Clinical stage is more important for prognosis vs. subtype.
Subtype also can affect prognosis:
- Lymphocyte-rich form of the disease has the best prognosis
- Lymphocyte/depleted form has worse prognosis (often presents with disseminated disease)
- Strong stromal/lymphocytic response against the Reed-Sternberg cells suggests a better response.
WAS THERE A WAY TO PREVENT IT?
No clear way to prevent this condition.
WHAT ELSE ARE WE WORRIED ABOUT?
Anemia of chronic disease is thought to be sometimes caused by HL
Minimal change disease: disease of the kidney that causes nephrotic syndrome (leukocyte disorder that results in excessive protein loss in the urine). Can check the patient’s urine for proteins.
OTHER HY FACTS?
Bimodal distribution: young adults and older individuals above 55
Leukemic phase does not really occur (high number of WBCs in the peripheral blood)
Page Updated: 01.13.2016