OVERVIEW
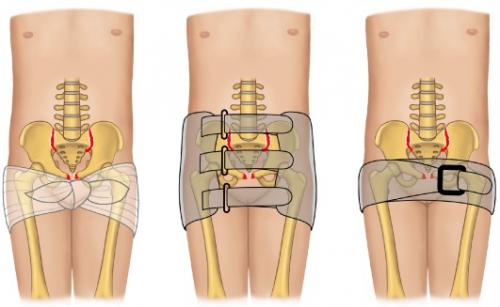
This page elaborates on how to properly place a pelvic binder on patients who have a pelvic fracture. While it is not an overly complicated topic, it can be nuanced. In most cases, placing a pelvic binder can provide significant benefit, and there rarely will be a contraindication to its placement. Pelvic binders can help stabilize the fracture anatomically AND can help control bleeding in the pelvis (by applying pressure and tamponading bleeding vessels by decreasing the potential space in the pelvis). In this way the judicious application of a pelvic binder can stabilize the patient both hemodynamically and anatomically.
The issue with placing a pelvic binder early on is that it can impede certain components of the physical exam, and can alter the anatomy of the fracture on imaging. It is for this reason that when possible the placement of a pelvic binder is delayed until the physical exam evaluation for damage to the vagina/uterus/urethra/bladder is quickly completed (more on that below). With this in mind, especially in a hemodynamically unstable patient, the binder may be placed before some of these exam components are completed.
Ideally before the pelvic binder is placed the urethra, vagina, and rectum will be examined properly (explained more below in the secondary survey): this can be done very quickly right before the binder is placed.
Once the binder is placed it is important to limit any reason that it will need to be taken off UNTILL the patient has been taken to the OR/IR suite for treatment.
Page Updated: 03.04.2018