Page Contents
WHAT IS IT?
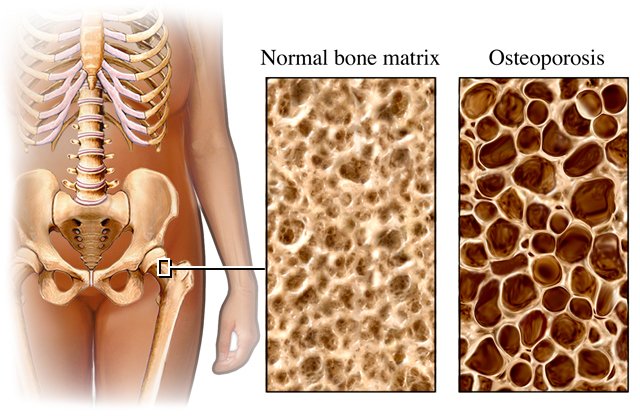
Osteoporosis does not have only one specific definition, but generally refers to the loss of bone (trabecular/spongy bone mass) by a patient. It is decreased density in bone that has retained normal bone architecture. Primary osteoporosis is classified in the following manner:
- Type 1 refers to post-menopausal osteoporosis (increased bone resorption due to decreased estrogen levels)
- Type 2 refers to “senile” osteoporosis that affects both men and women in older age (>70 years of age).
Many things can cause osteoporosis including:
- Prolactinoma
- Prednisone (glucocorticoid) toxicity
- Heparin
- Estrogen deficiency (menopause)
- Cushing syndrome
- Anticonvulsants
- Anticoagulants
- Hyperthyroidism
- Thyroid replacement therapy
WHY IS IT A PROBLEM?
The loss of this bone mass leads to generalized bone weakness (porous bone), and a higher incidence of fracture.
WHAT MAKES US SUSPECT IT?
Risk factors: postmenopausal women, older age (> 65-70 years old), caucasian/asian descent, small body frame
Common clinical presentation can include the following:
- Acute back pain
- Loss of height
- Kyphosis
Common presenting fractures can include:
- Head of femoral neck
- Distal radius (Colles fracture)
- Hip
- Vertebral fracture

HOW DO WE CONFIRM A DIAGNOSIS?
Serum analysis is not diagnostic for primary osteoporosis because it is not defined by changes in serum calcium, phosphate, ALP, or PTH levels (these values are usually within the reference range).
- That being said, high PTH can sometimes cause SECONDARY osteoporosis the above serum findings only refer to PRIMARY osteoporosis.
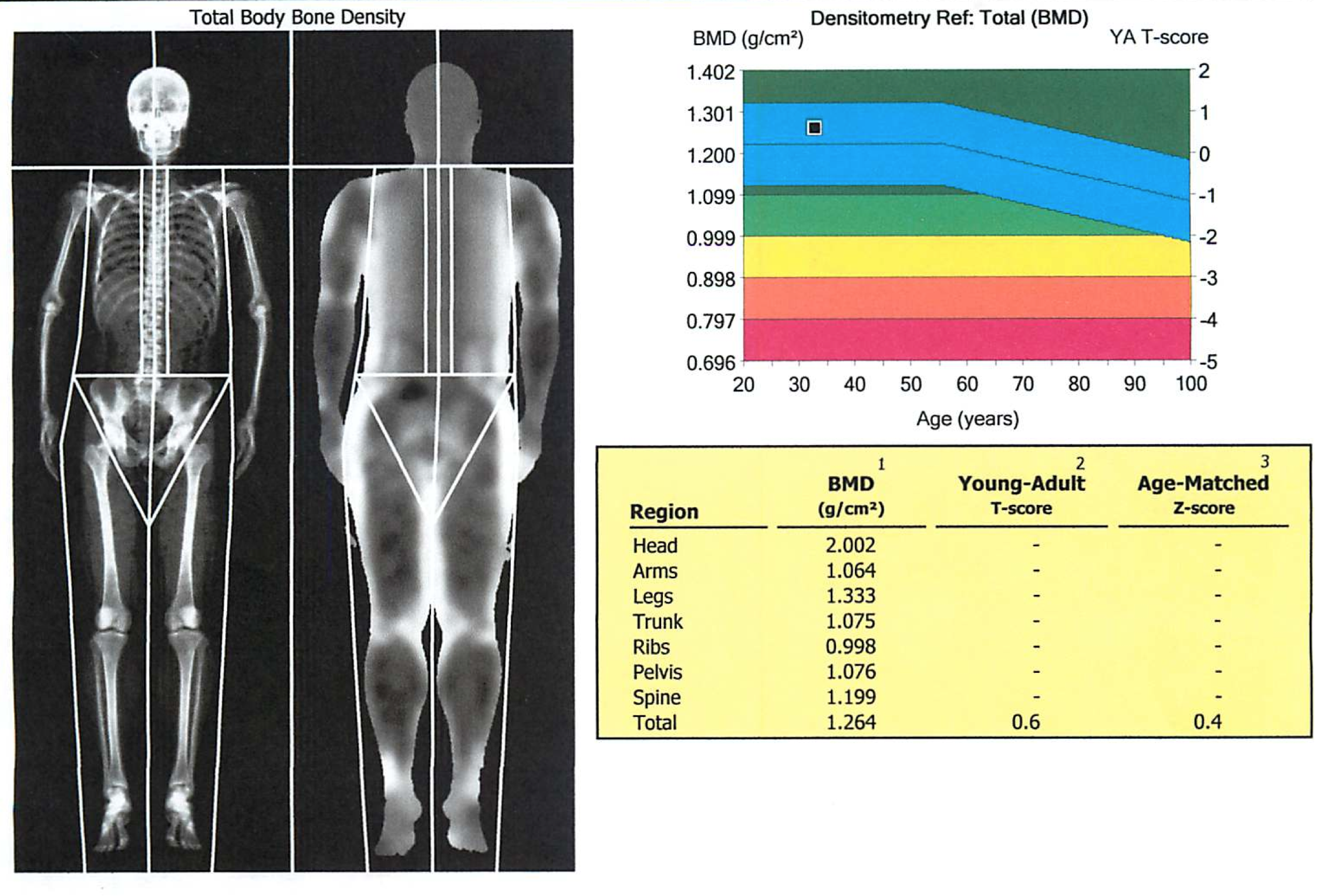
Dual-energy X-ray (DEXA): this is a bone mineral density test. A T-score of ≤ −2.5 is typically diagnostic.
- A T-score compares one’s bone density to that of a young adult (ideal control).
- A Z-score compares one’s bone density to an age, sex, race, weight matched control.
*Both T and Z scores are measures of the number of standard deviations away from the control mean.
HOW DO WE TREAT IT?
Supplementation of calcium and vitamin D can help slow bone deterioration.
Bisphosphonates (alendronate): these are pyrophosphate analogs that bind hydroxyapatite in bone. They are ultimately taken up by osteoclasts, at which point they inhibit their activity (and can induce apoptosis).
Teriparatide: this is a recombinant PTH analog that increases osteoblast activity.
Denosumab is an antibody targeting the RANK ligand. This inhibits osteoclast maturation (and mimics the action of osteoprotegerin)
Selective estrogen receptor modulators (SERMs) have been approved to treat osteoporosis in post-menopausal women. These include medication such as tamoxifen and raloxifene that increase estrogen signaling pathways.
Thiazide diuretics (ex. HCTZ) can be used to increase the re-uptake of calcium by the nephron
HOW WELL DO THE PATIENTS DO?
Patients are (as discussed before) at higher risk for fractures. The results of a DEXA scan are a very good prognostic marker for fragility fracture risk (the lower the bone density => higher risk for fracture).
WAS THERE A WAY TO PREVENT IT?
Calcium and vitamain D supplementation can be used as prophylaxis for this condition.
Weight bearing exercise has also been shown to help keep bone density increased in patients.
WHAT ELSE ARE WE WORRIED ABOUT?
*Any fracture in general!
Vertebral compression fractures are common in patients with osteoporosis given that they are weight bearing bones.
Continued glucocorticoid usage is contraindicated because it will worsen the osteoporosis.
OTHER HY FACTS?
Hormone replacement therapy (such as estrogen replacement in menopause) can help address osteoporosis by replacing estrogen (which in turn decreases osteoclast activity).
Peak bone mass is achieved at the age of 30 and depends upon the following factors:
- Genetics (i.e. vitamin D receptor variants)
- Diet
- Exercise
Homocystinuria is the deficiency of metabolizing the amino acid methionine, and it can preset with osteoporosis.
Gaucher disease is a lysosomal storage disorder (deficiency of glucocerebrosidase) that can present with osteoporosis.
Renal osteodystrophy is an alteration of bone morphology due to chronic kidney disease that typically presents with osteoporosis.
Multiple Myeloma can deposit antibodies in the bone leading to a different form of “osteoporosis”
Calcitonin in theory should help with osteoporosis
FURTHER READING
Page Updated: 02.23.2016