Page Contents
OVERVIEW
This guide is dedicated to covering the topic of how to approach treating patients who have diabetes (type 1/type 2).
WHAT IS IT?
While we will not get too in detail regarding all the differences between different types of diabetes, fundamentally diabetes is defined by dysregulation of blood sugar as a result of impaired insulin signaling.
Patients are not able to clear glucose from their circulating blood on their own, and as a result, will have elevated levels of blood sugar. This increase in blood sugar can damage various structures within the body, leading to a wide host of complications.
HOW DO WE DIAGNOSE IT?
Type 2 DM Diagnostic Criteria (American Diabetes Association, source): one of these 4 criteria must be met on TWO separate days
- Random plasma glucose ≥ 200 mg/dL in tandem with symptoms of diabetes (polyuria, polydipsia)
- Fasting plasma glucose ≥ 126 mg/dL
- Glucose tolerance test: two-hour plasma glucose level ≥ 200 mg/dL after 75 g of oral glucose administered
- HbA1c of 6.5% or higher
Pre-diabetes criteria (source):
- Fasting glucose: 100-125 mg/dL
- Glucose tolerance test: two-hour plasma glucose level 140-199 mg/dL after 75 g of oral glucose administered
- HbA1c of 5.7–6.4%
WHAT IS THE BASE TREATMENT GOAL?
The fundamental treatment goal of diabetes is not complicated. Controlling blood sugar truly is the endgame for managing this disease. As is the case with anything else, there really are a finite number of options that we have at our disposal to accomplish this goal.
The role of lifestyle changes: while this element is often glossed over in medicine, it is arguably the most critical.
- Diet: perhaps the most important element of all, before the glucose enters the blood it must come from some dietary source. Eating food that has a low glycemic index AND low net sugars can go a long way in helping make diabetes manageable.
- Exercise: exercise has been shown to clear blood glucose from a non-insulin mediated mechanism. This is very advantageous to diabetes patients.
The role of glucose controlling medications: this aspect of diabetes management can get quite confusing, so we will touch on it briefly for now. Fundamentally the principle is that we leverage different biological systems within the body to help control blood sugar.
- Insulin: the role of insulin can vary depending on the nature of the diabetes. Given that a large element of diabetes revolves around insulin signaling complications, it is very intuitive to try and restore this signaling axis in patients with diabetes.
- Non-insulin diabetes medications: this is a vast topic. The main idea to get across right now is that there are MANY options when it comes to controlling blood sugar using non-insulin medications.
WHAT IS THE SPECIFIC TARGET?
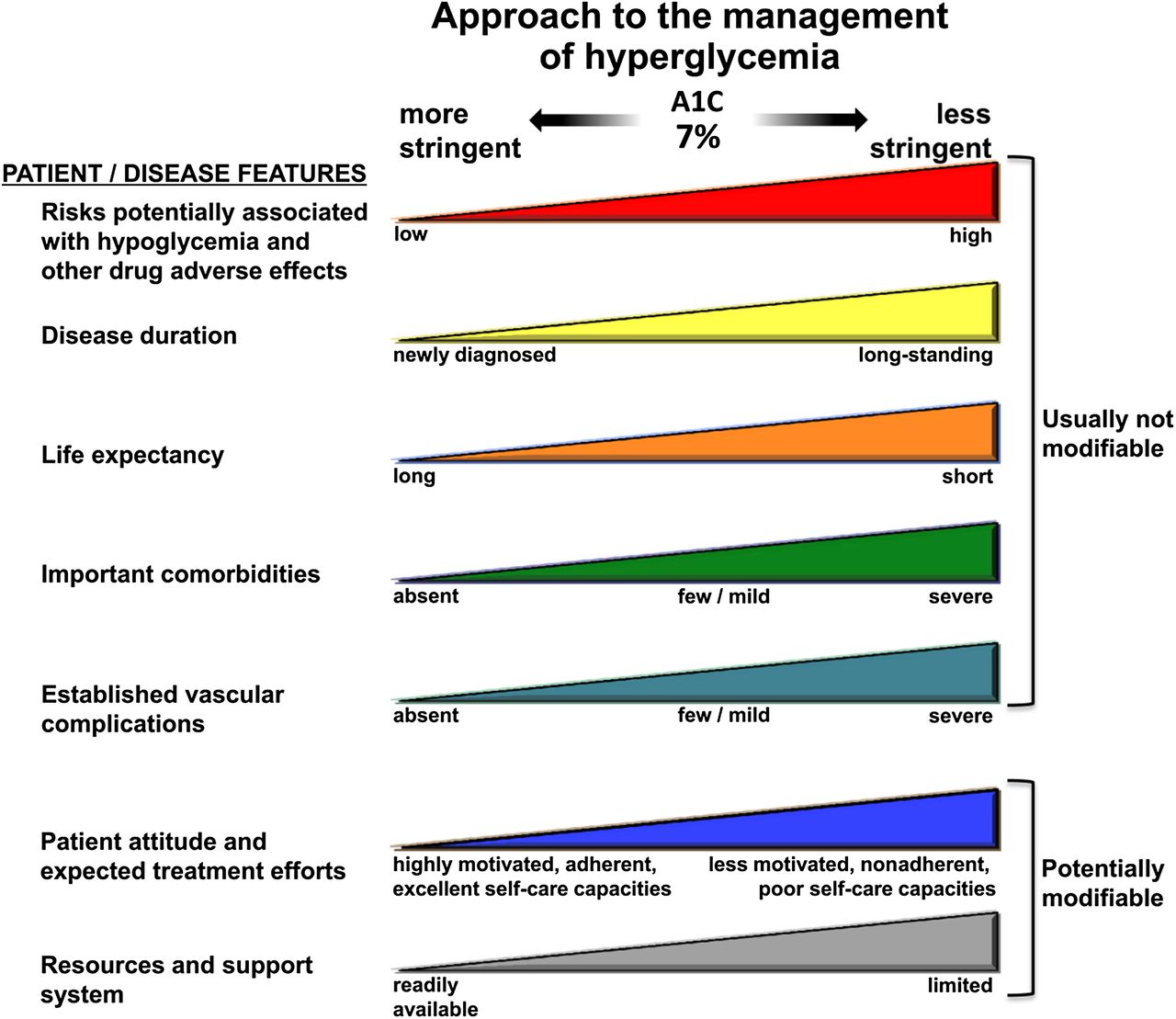
Lowering the patient’s HgA1C is the functional target of treating diabetes. Exactly how much it should be lowered will depend on a few different factors. With this in mind we can use a HgA1C of less then 7% as a general target (however many factors may come into play when modifying this on a patient per patient basis.
Page Updated: 08.16.2016