Page Contents
- 1 OVERVIEW
- 2 WHAT IS AN OUTPATIENT COMMUNITY ACQUIRED PNEUMONIA?
- 3 HOW DO WE DECIDE THAT A PATIENT HAS A COMMUNITY ACQUIRED PNEUMONIA THAT WILL BE TREATED IN THE OUTPATIENT SETTING?
- 4 WHAT ARE THE LIKELY PATHOGENS THAT WILL COMMONLY CAUSE COMMUNITY ACQUIRED PNEUMONIA?
- 5 STARTING ANTIBIOTIC THERAPY: WHAT SHOULD BE DONE BEFORE PRESCRIBING MEDICATIONS?
- 6 STARTING ANTIBIOTIC THERAPY: WHAT ARE THE TREATMENT OPTIONS?
OVERVIEW
This page is dedicated to providing a practical guide to how one should pick the correct antibiotic(s) to use in the setting of a outpatient community acquired pneumonia.

WHAT IS AN OUTPATIENT COMMUNITY ACQUIRED PNEUMONIA?
In thinking about this phrase we can break it down into a few different sections.
- What type of infection? This refers to an infection within the lungs (pneumonia)
- In what setting did the patient acquire the infection? This will help inform what types of pathogens are most likely to have caused the infection (more on this below).
- How in what setting will the patient be managed? The severity of the infection in this case allows for patients to be treated in the outpatient setting (which will influence how aggressively the patients are treated).
**While they may seem tedious now, all of the above components directly influence the management and clinical course of the patient, which is why they are worth mentioning!**
HOW DO WE DECIDE THAT A PATIENT HAS A COMMUNITY ACQUIRED PNEUMONIA THAT WILL BE TREATED IN THE OUTPATIENT SETTING?
There are a few important components to appreciate in categorizing a patient with a community acquired pneumonia that will be managed in the outpatient setting:
Patient History:
- Chief complaint: can be that of a cough and/or a fever
- Onset: patient should not be living in a nursing home or recently have been in the hospital when the contracted the illness for this to be a true community acquired pneumonia.
- Severity: overall this patient should present in a relatively stable fashion in order to be managed in the outpatient setting.
Physical Exam:
- Vitals can reveal a fever and some other abnormalities (however should be relatively stable if the patient will be treated in the outpatient setting).
- Respiratory exam can be notable for crackles, decreased breath sounds, increased fremitus, and dullness to percussion.
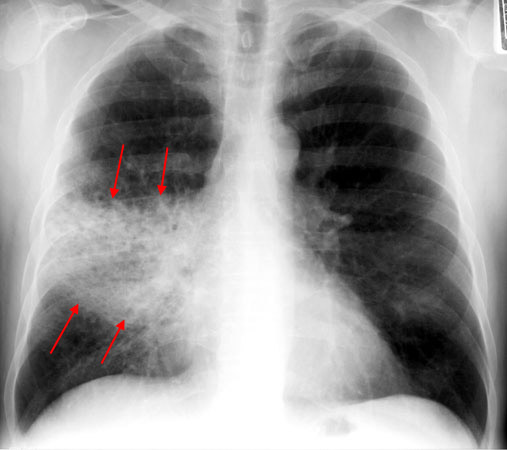
Chest X-Ray:
In thinking about pneumonia it is important to appreciate that very often a suspected diagnosis will be made using a chest X-ray.
WHAT ARE THE LIKELY PATHOGENS THAT WILL COMMONLY CAUSE COMMUNITY ACQUIRED PNEUMONIA?
Before talking about specific antibiotics we need to appreciate the pathogens that will most commonly cause community acquired pneumonia (because these dictate what treatments are worth giving!). The below are the most common bacterial pathogens that are responsible for commonly causing this type of pneumonia.
- Streptococcus pneumoniae
- Haemophilus influenzae
- Chlamydophila pneumoniae
- Legionella pnuemophilia
- Mycoplasma pneumoniae
- Staphylococcus aureus
Later when we discuss treatment options, let us appreciate that guidelines are crafted to try and cover the above pathogens!
Some hard “truths” to realize about the causal pathogen of community acquired pneumonia:
- A large percentage of community acquired pneumonias are caused by viral pathogens: these will of course not be cured using antibiotics.
- A large fraction of the time the causative pathogen is never identified in community acquired pneumonia: While cultures may be collected before that start of treatment, it is important to appreciate that bacterial cultures take time to grow, often get contaminated, and that they may not always identify a single pathogen. Figuring out the exact pathogen responsible for the pneumonia is not always a practical task!
STARTING ANTIBIOTIC THERAPY: WHAT SHOULD BE DONE BEFORE PRESCRIBING MEDICATIONS?
Recent antibiotic usage? It is important to ask all patients who are about to start antibiotic therapy if they have used any antibiotics in the recent past. The spirit behind this question point is that it is generally not advantageous to give the same course of antibiotics in patients back to back (in thinking about drug resistance).
Collect cultures: sputum cultures might be collected in patients who are going to be managed in the outpatient setting (blood cultures make much less logistical sense as a patient with suspected bacteria will likely not be managed outpatient). It is possible that the causative pathogen may be identified using this culture method (although some may forgo collecting the cultures as it might not change the clinical management of the patient).
STARTING ANTIBIOTIC THERAPY: WHAT ARE THE TREATMENT OPTIONS?
It is important to appreciate that their are two major sets of guidelines that impact the types of antibiotics that are prescribed in an outpatient setting.
American IDSA Guidelines: these guidelines are geared to have more coverage of different types of community acquired pathogens (such as Chlamydophila pneumoniae, Legionella pnuemophilia, and Mycoplasma pneumoniae) BUT do a worse job in treating the most likely pathogen (Streptococcus pneumoniae)
No recent antibiotic therapy: this setting the following options are commonly used
- Macrolides: Azithromycin is a very commonly used medication.
- Doxycycline is an older medication but also can be effective.
Recent antibiotic therapy:
- Respiratory fluoroquinolone: Moxifloxacin, Levofloxacin, Gemifloxacin are all options
- Macrolide (i.e. Azithromycin)+ high dose amoxicillin
- Augmentin
European Guidelines: the treatment practices in Europe are tailored to treating the most likely pathogen (Streptococcus pneumoniae) more effectively, at the cost of not covering some of the other pathogens that are “atypical” causes of pneumonia(such as Chlamydophila pneumoniae, Legionella pnuemophilia, and Mycoplasma pneumoniae).
- Penicillin: superior to macrolides or doxycycline for Streptococcus pneumoniae coverage
- Amoxicillin: superior to macrolides or doxycycline for Streptococcus pneumoniae coverage
- AVOID fluoroquinolones as above therapies seem to work just as well.
Page Updated: 09.13.2016