Page Contents
- 1 OVERVIEW
- 2 WHAT ARE PAP SMEARS?
- 3 WHY DO WE DO THEM?
- 4 HOW IS IT DONE?
- 5 WHAT IS THE ROUTINE TESTING SCHEDULE FOR PAP SMEARS?
- 6 WHAT ARE THE POSSIBLE RESULTS OF A PAP SMEAR?
- 7 WHAT TO DO NEXT: NEGATIVE FOR INTRAEPITHELIAL LESION OR MALIGNANCY
- 8 WHAT TO DO NEXT: ASC-US
- 9 WHAT TO DO NEXT: LSIL
- 10 WHAT TO DO NEXT: ASC-H
- 11 WHAT TO DO NEXT: HSIL
- 12 WHAT TO DO NEXT: SQUAMOUS CELL CARCINOMA
- 13 WHAT TO DO NEXT: AGC-NOS/AGC-ENDOCERVICAL
- 14 OTHER REFERNCES
OVERVIEW
This page is dedicated to going over the clinical utility of pap smears. A large purpose of this page will be clarifying when a colposcopy should be performed. In essence, this page aims to answer the question: What is the threshold deciding to perform a colposcopy on a patient?
Make sure to read the stepwards.com disclaimer before using the content of the page below.
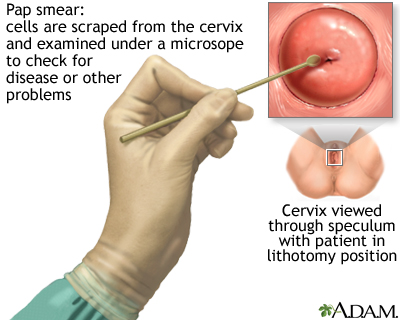
WHAT ARE PAP SMEARS?
A Papanicolaue (Pap) smear refers to a screening test that collects cells from the female cervix for cytological analysis. There are a few different ways in which the cells can be collected/prepared, however fundamentally the concept remains the same.
Pap smears can be done in isolation or can be conducted along side an HPV screen (referred to as co-testing).
WHY DO WE DO THEM?
Screen for malignancy: Pap smears are generally done to screen for the presence of cervical cancers/or pre-malignant lesions in the cervix that may become cancerous in the future. Other information can be gathered form the test, however most often it is done to assess for possible/current malignancy in the cervix.
In essence the Pap smear is used (sometimes with HPV testing) to decide if more investigation (i.e. colposcopy) is needed to determine if a patient has a pre-cancerous or cancerous condition. A pap smear on its own rarely can be used diagnostic, however it will dictate if the patient requires further workup.
HOW IS IT DONE?
WHAT IS THE ROUTINE TESTING SCHEDULE FOR PAP SMEARS?
The below section is not completely comprehensive, but provides some of the highlights to keep in mind regarding what a routine Pap smear schedule may refer to. More information can be found in these guidelines. Fundamentally, the age of the patient will dictate routine screening practices.
Patients below 21 years of age:
Most all guidelines agree that patients younger then 21 years of age should not receive Pap smears, regardless of when they became sexually active, or other risk factors. The exception to this general rule are patients who are immunocompromised (which warrant that patients begin cervical cancer screening at the onset of sexual intercourse). Examples of this patient demographic include:
- HIV infected patients
- Patients with systemic lupus erythematous
- Transplant patients
- Patients on immunosuppressants
Generally these patients should receive screens every 6 months for (2x) and then be screened annually after that point.
Patients ages 21-29:
Patients in this age range should receive a Pap smear every 3 years. It is not recommended that patients below the age of 30 get HPV testing.
Patients ages 30-64:
Patients in this age range may have a few different options for testing that may seem a bit confusing. At age 30 it generally can be a good idea to receive 1 Pap smear/HPV co-test and use this to determine future screening practices.
If the co-test is completely negative patients may have the option of having repeat co-tests every 5 years.
If the co-test is positive routine screening in the future may require a shorter testing interval (repeat pap smears every 3 years +/- HPV co-testing).
Patients above 65 years of age:
It is generally recommended to stop screening altogether. There are some exceptions to this rule that can include:
- Increased risk for malignancy: this can include a history of abnormal screening, current smoker or history of smoking, unknown screening history, previous HPV-related disease, new partners, immunocompromised, in utero diethylstilbestrol exposure.
- Absence of adequate prior screening: in the absence of two negative consecutive co-tests or three negative Pap tests within the past 10 years, (with the most recent test within the previous five years) it may be worth considering continue screening behind the age of 65.
- History of high grade dysplasia or worse: often warrants continued screening.
WHAT ARE THE POSSIBLE RESULTS OF A PAP SMEAR?
After a pap smear is ordered and evaluated by a pathologist there are a finite number of different results that can be reported back. Many common results that are reported are listed below (although the list is not entirely comprehensive). The exact terminology used in lab reports may vary by practice location. Information below is from the Bethesda System Terminology.
Normal results:
Negative for intraepithelial lesion or malignancy: this is the most “normal” result and essentially means that no cells collected during the pap smear were suspicious for current or future malignancy.
Abnormal results: squamous cell abnormalities
Atypical squamous cells of undetermined significance (ASC-US): This is a finding that does not have much closure, and warrants further investigation. In essence it means that atypical (non-normal) squamous cells were found, however that the pathologist was unable to clearly decide if they were concerning for malignancy or not. These cells do not resemble squamous intraepithelial lesion cells.
Low-grade intraepithelial lesion (LSIL): this pap smear finding means that cervical cells were found that are mildly abnormal. These changes are comparatively mild (hence the name “low-grade”) and may be caused by HPV infection (can be reversible).
Atypical squamous cells in which a high-grade squamous intraepithelial lesion cannot be excluded (ASC-H): This result means that the cells analyzed by the pathologist consisted of a mixture of true high-grade squamous intraepithelial lesion cells and other cells that might mimic this type of lesion. This finding is concerning for a high-grade squamous intraepithelial lesion.
High-grade squamous intraepithelial lesion (HSIL): this finding suggests more serious changes in the cervical cells (compared to LSIL). This finding is much more likely to be caused by either a pre-cancerous or cancerous state.
Squamous cell carcinoma: based upon this Pap smear result, there is a high likelihood that the patient currently has squamous cell carcinoma.
Abnormal results: glandular cell abnormalities
Atypical glandular cells not otherwise specified (AGS-NOS):
Atypical glandular cells, endocervical (AGS-endocervical):
Atypical glandular cells, endometrial (AGS-endometrial):
Atypical glandular cells, favor neoplastic (AGS-favor neoplastic):
Endocervical adenocarcinoma in situ (AIS):
Adenocarcinoma:
WHAT TO DO NEXT: NEGATIVE FOR INTRAEPITHELIAL LESION OR MALIGNANCY
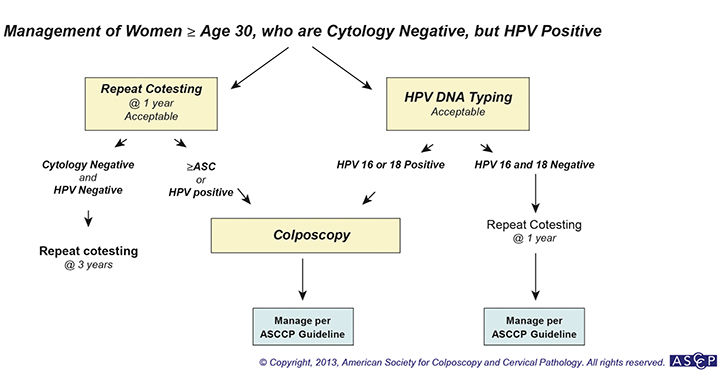
Generally speaking, this type of Pap smear result (without a past history of abnormal pap smear results) will result in patient’s resuming a routine screening schedule (see above).
Once caveat of this will be patients who are 30 years of age or above who have a normal Pap smear, but have a positive HPV result.
WHAT TO DO NEXT: ASC-US
If a patient receives a pap smear result of ASC-US, then the next steps in managment depend on the age of the patient:
Patients 21-24 years of age: should repeat their pap smear in 12 months. The results of this pap smear will dictate what is done next.
Repeat Pap is negative, ASC-US, or LSIL: then the Pap smear should be repeated again in 12 months.
- If negative then patient should repeat pap smear again in 12 months. If this too is negative then the patient can return to routine screening.
- If any of the repeat tests have ASC-US or a more severe abnormality then colposcopy should be performed.
Repeat Pap is ASC-H, HSIL, or atypical glandular cells: colposcopy should be performed.
Patients 25 years of age or older: should have HPV testing. The results of the HPV test will decide what happens next.
Patients who are HPV negative should have repeat co-testing (Pap smear and HPV testing) again in 3 years.
Patients who are HPV positive should have a colposcopy performed.
WHAT TO DO NEXT: LSIL
Patients with a pap smear result of LSIL will have different management based upon their age.
Patients 21-24 years of age: should repeat their pap smear in 12 months. The results of this pap smear will dictate what is done next.
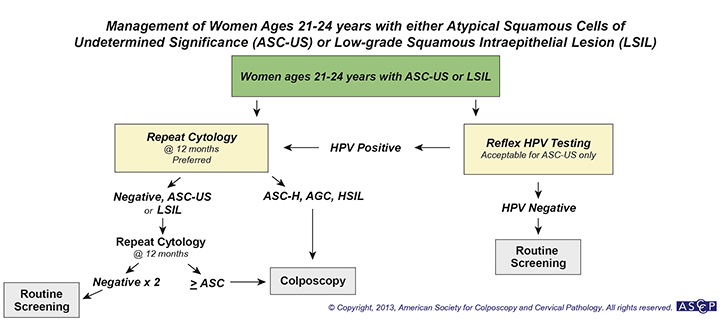
Repeat Pap is negative, ASC-US, or LSIL: then the Pap smear should be repeated again in 12 months.
- If negative then patient should repeat pap smear again in 12 months. If this too is negative then the patient can return to routine screening.
- If any of the repeat tests have ASC-US or a more severe abnormality then colposcopy should be performed.
Repeat Pap is ASC-H, HSIL, or atypical glandular cells: colposcopy should be performed.
Patients 25-29 years of age:
In this age group colposcopy should be performed (regardless of HPV status).
Patients 30 years of age or older: should be managed by their HPV status (typically this age group should have received an HPV test during the time of the Pap smear).
Patients who are HPV negative: these patents should have repeat HPV/pap smear co-testing in one year.
- If co-testing results are negative then co-testing should be repeated in three years
- If co-testing results are positive or HPV status is unknown then colposcopy should be performed.
Patients who are HPV positive/HPV status unknown: then colposcopy should be performed.
WHAT TO DO NEXT: ASC-H
With the finding of ASC-H (regardless of age group) patients should have a colposcopy performed.
WHAT TO DO NEXT: HSIL
Patients with this finding have slightly different options depending on their age.
Patients 21-24 years of age:
In this age group patients should have a colposcopy performed
Read more here on what to do next.
Patients 25 years of age or older:
In this age group patients have 2 options:
- Perform a colposcopy
- Have an immediate loop electrosurgical excision procedure performed (should not be done in patients below 25 years of age or pregnant women).
WHAT TO DO NEXT: SQUAMOUS CELL CARCINOMA
WHAT TO DO NEXT: AGC-NOS/AGC-ENDOCERVICAL
Both AGC-NOS and AGC-endocervical are managed based upon the findings
OTHER REFERNCES
UpToDate: Evaluation of atypical squamous cells (ASC-US and ASC-H)
UpToDate: Evaluation of low-grade squamous intraepithelial lesions (LSIL)
Page updated: 07.27.2016