Page Contents
- 1 OVERVIEW
- 2 IS THIS A CENTRAL OR PERIPHERAL NERVOUS SYSTEM ISSUE?
- 3 CNS VS. PNS: MOTOR PATHWAYS
- 4 CNS VS. PNS: SENSORY PATHWAYS
- 5 CNS VS. PNS: CRANIAL NERVES
- 6 CNS: DOES THE PATIENT HAVE ISSUES REMAINING CONSCIOUS?
- 7 CNS: DOES THE PATIENT HAVE DIFFICULTY COORDINATING MOVEMENTS?
- 8 CNS: DOES THE PATIENT HAVE DIFFICULTY INITIATING OR STOPPING VOLUNTARY MOVEMENTS?
- 9 CNS: DOES THE PATIENT HAVE APHASIA/LANGUAGE DEFICITS?
- 10 CNS: DOES THE PATIENT HAVE PERSONALITY CHANGES?
- 11 CNS: ARE THERE SYMPTOM PATTERNS THAT CAN HELP LOCALIZE THE LESION?
- 12 PNS: WHERE IN THE PERIPHERAL NERVOUS SYSTEM CAN THE ISSUE BE?
- 13 PNS: DO KEY SPINAL ROOTS SEEM INVOLVED?
- 14 ACKNOWLEDGMENTS
OVERVIEW
This guide is meant to be used after one has determined that they are very likely dealing with a neurological issue. The purpose of this guide is to aid you in deciding which area of the body to image in order to identify the casual lesion. It is not meant to necessarily be used linearly, however the order set forth below is designed to try and be as inclusive and efficient as possible.
This guide also assumes that a full neurological exam has been completed that includes: mental status exam, cranial nerve exam, and the supporting components of the neurological exam.
IS THIS A CENTRAL OR PERIPHERAL NERVOUS SYSTEM ISSUE?
Perhaps one of the most useful distinctions that can be made initially when characterizing neurological issues is if the complications arise in the central nervous system (CNS) or the peripheral nervous system (PNS).
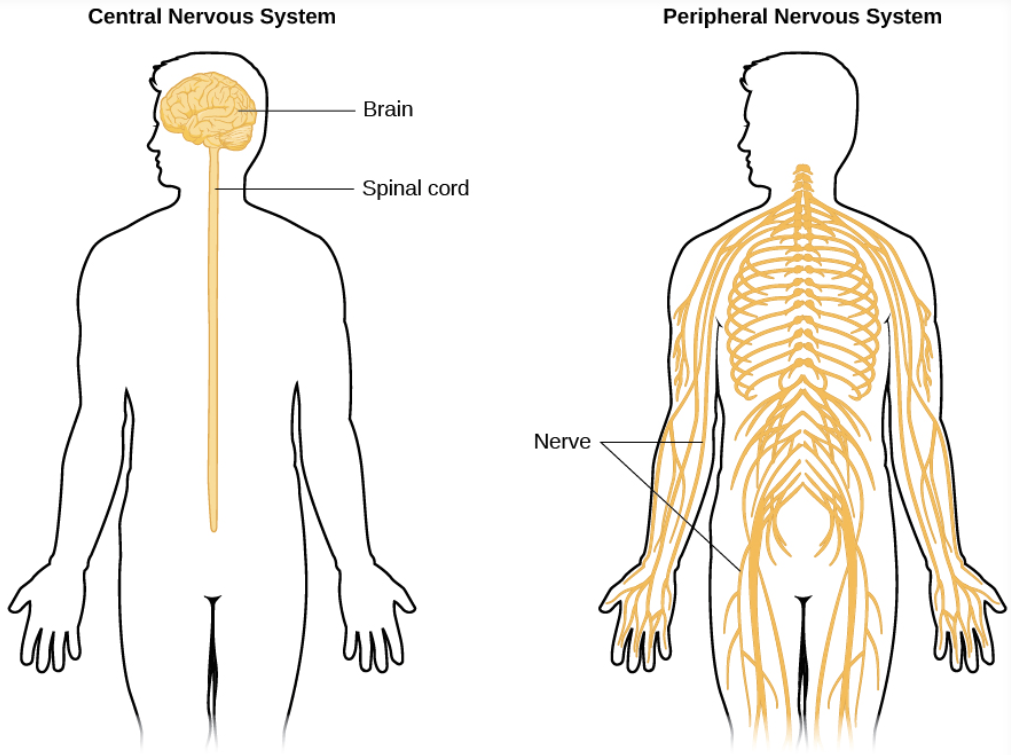
What makes us suspect CNS involvement? If a patient has symptoms relating to any of the following components, then some aspect of their central nervous system is MUST be impaired (if it is neurological issue):
- Level of consciousness
- Issues coordinating movements (cerebellum)
- Difficulty initiating voluntary movement (basal ganglia)
- Complications with speech and language
- Behavioral/personalty changes
Which processes can be either CNS/PNS? If the following symptoms are observed in patients then both CNS and PNS issues might be responsible. Further characterization will be needed for:
- Motor pathway deficits
- Sensory pathway deficits
- Visual complications/disturbances*
- Hearing issues*
- Impaired sense of smell*
- Taste impairment*
- Facial sensation complications*
- Movement of facial muscles*
*These processes involve the cranial nerves
CNS VS. PNS: MOTOR PATHWAYS
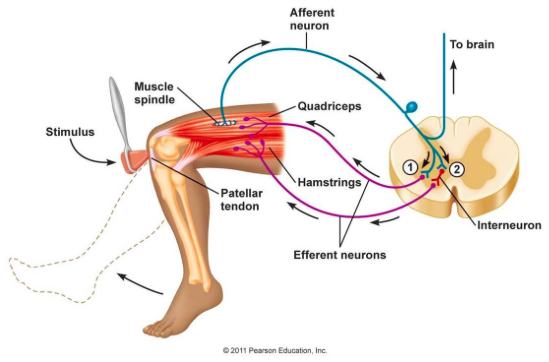
There are a few key findings that can help differentiate between lesions that affect the central nervous system (upper motor neurons) and the peripheral nervous system (lower motor neurons). Keep in mind issues with either neuron can cause weakness in the muscles.
Upper motor neuron issues (CNS):
- Hyperflexia (increased reflexes)
- Babinksi sign
- Increased tone/spasticity (velocity dependent resistance to movement)
- No muscle atrophy (at first)
Lower motor neuron issues (PNS):
- Hypoflexia (diminished reflexes)
- Atrophy of muscles
- Fasciculations (twitches)
- Cramps
CNS VS. PNS: SENSORY PATHWAYS
Dermatomal loss of sensation can be suggestive of damage to peripheral nerves that arise from specific spinal roots (PNS implicated).
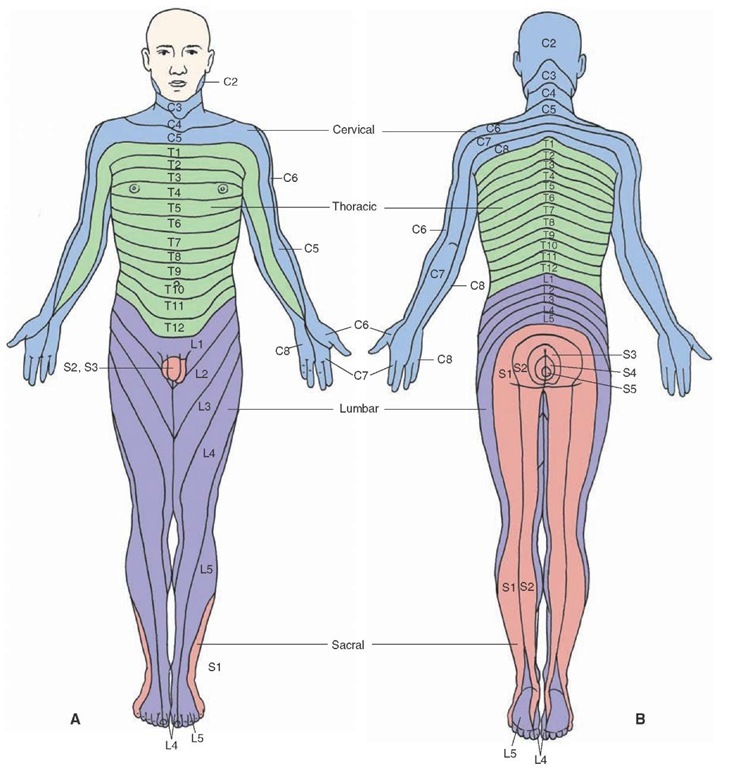
Non-dermatomal loss of sensation can be either a CNS or PNS issue. A nerve plexus or individual nerves can be damaged leading to non-dermatomal losses (PNS implicated), or entire regions of the body can lose sensation due to central lesions (CNS can be implicated).
CNS VS. PNS: CRANIAL NERVES
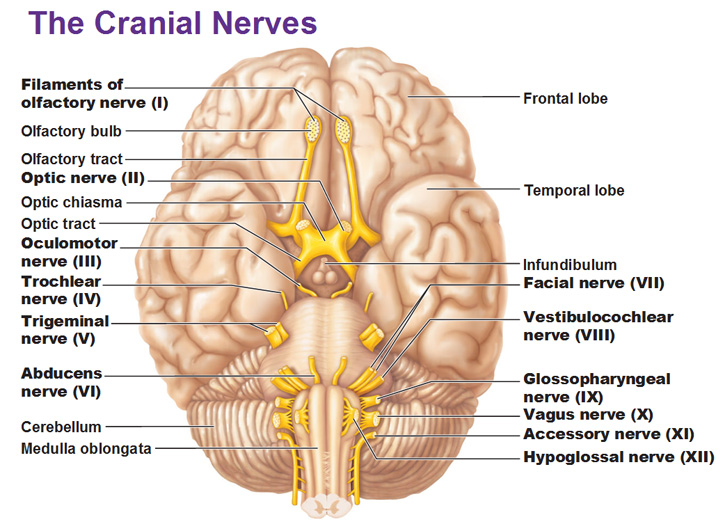
Remember that vision, eye movmeents, smell, taste hearing, facial movement and facial sensation are controlled by cranial nerves. Symptoms with their involvement can be caused by issues either in the CNS or in the actual cranial nerves themselves (which are part of the PNS). More information on each cranial nerve can be found here. Ultimately the clinical presentation of the patient combined with their constellation of neurological symptoms can help contextualize if cranial nerve deficiencies are peripheral or central in origin.
It is also important to remember that some of the cranial nerve nuclei are found at different levels of the brainstem (CNS).
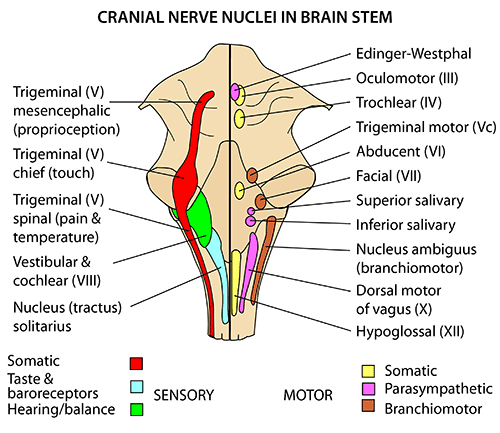
Below are the general locations of the cranial nerves on gross examination. While the nuclei are found within the CNS, the nerves themselves are incited by Schwann cell myelin and subject to peripheral disease (such as Guillain-Barre). As a result one must consider them to be a part of the CNS.
CNS: DOES THE PATIENT HAVE ISSUES REMAINING CONSCIOUS?
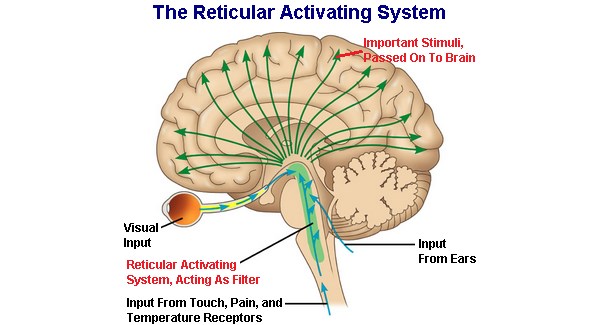
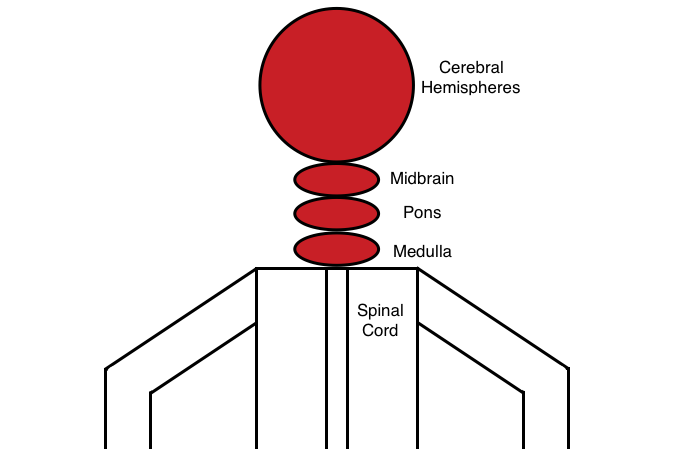
If the patient is unable to retain consciousness then it is very likely that some issue is present with the reticular activating system (RAS) that is found in the brainstem. The RAS is responsible for keeping individuals awake, and this very easy to detect facet of the neurological exam can help save precious time in addressing a serious issue. Many different things can cause issues with the RAS including direct damage and even increased intracranial pressure. The brain stem (and likely the cerebral hemispheres) should be imaged.
CNS: DOES THE PATIENT HAVE DIFFICULTY COORDINATING MOVEMENTS?
The coordination of multiple movements involve the action of the cerebellum. Patients who exhibit the following symptoms might have damage/impairment of their cerebellum:
- Wide based gait
- Nystagmus
- Intention tremor
*It is important to realize that other symptoms (such as muscle weakness) can be mistaken for issues cerebellar issues (ex. weakness in the legs can lead to a wide based gait.
CNS: DOES THE PATIENT HAVE DIFFICULTY INITIATING OR STOPPING VOLUNTARY MOVEMENTS?
The basal ganglia is the structure in the brain that is responsible for either initiating or inhibiting voluntary movements. Damage to this structure (or in the signaling pathways that regulate its activity) can lead to both the inability to have a desired movement/akinesia/bradykinesia (such as Parkinson disease) or uncontrollable flailing movements/hemiballismus (Huntington disease).
CNS: DOES THE PATIENT HAVE APHASIA/LANGUAGE DEFICITS?
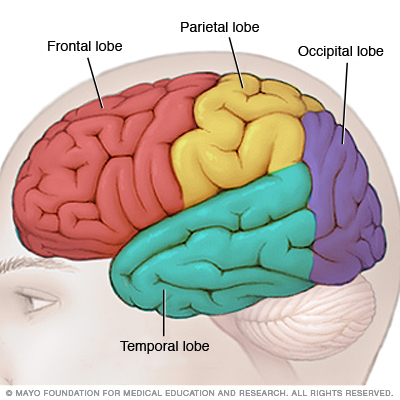
Aphasia refers to the lost ability to understand or express speech. Structures in the left hemisphere are important for language, and can be damaged in individuals who have difficulty producing/comprehending speech. There are four prototypical aphasias that can sometimes be localized to specific regions of the cerebral cortex.
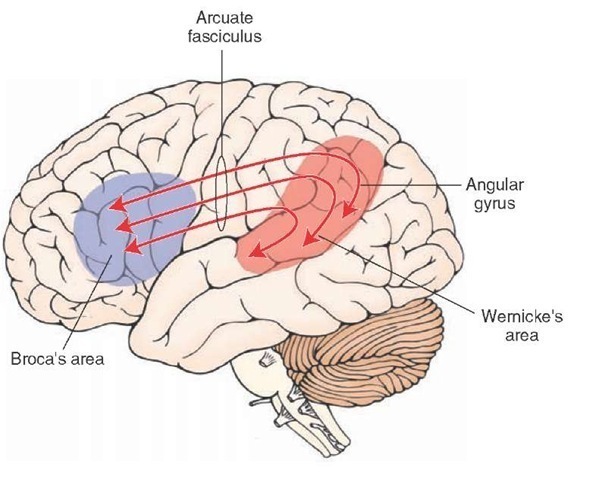
Broca’s Aphasia: is an issue with regards to expression (not comprehension). Patients are able to understand those that speak to them, however they are non-fluent in their speech. Involves the Broca’s area (motor)
Wernicke’s Aphasia: is a complication that stems from impaired comprehension by the patient. They are able to speak fluently, however typically use nonsensical words (and are unable to detect that they are speaking gibberish). Involves the Wernicke’s area (sensory)
Conduction Aphasia: patients are both fluent and have preserved comprehension, however are unable to accurately repeat back sentences that they hear. This involves the connections (arcuate fasciculus) between Broca’s area and Wernicke’s area.
Global Aphasia: fluency, comprehension, and reputation are all impaired in the patient. Can involve both Broca’s and Wernicke’s area (as well as the connections between them).
CNS: DOES THE PATIENT HAVE PERSONALITY CHANGES?
Behavioral changes that include personality, judgement, insight, emotions, and decision making (to include a few) might involve the frontal lobes of the brain.
CNS: ARE THERE SYMPTOM PATTERNS THAT CAN HELP LOCALIZE THE LESION?
Deficits of pathways in the head: no level of the spinal cord is responsible for innervating the head for motor or sensory pathways. Look above the spinal cord in the CNS for the underlying cause of the symptoms.
Cerebral hemispheres: looking at the homunculus can help us appreciate what types of lesions can bring about certain clinical symptoms.
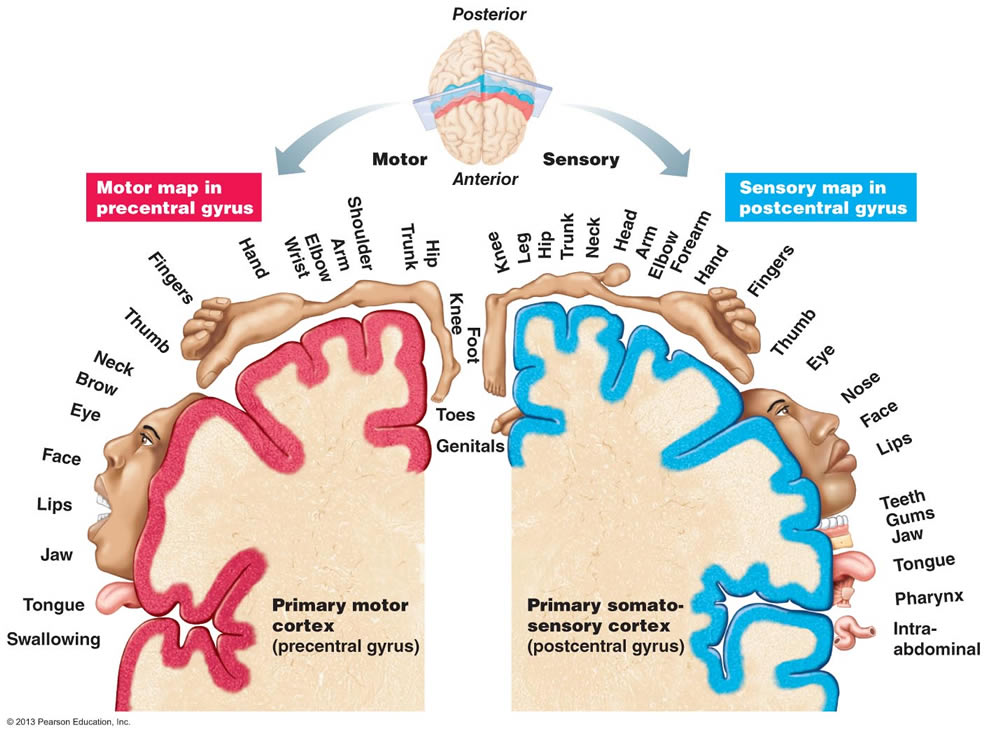
Arm involvement: much like the face, involvement of the arms in any way will require that a casual lesion be found at above the T3 level of the spine (given T2 is the last spinal root to innervate any structure in the arm). If your patient presents with any arm involvement (regardless of other symptoms) you must appreciate that at least one lesion must exist above T3 (either in the CNS or the periphery)
Opposing loss of facial and body sensation (pain/temperature): the pattern seen below suggests an issue between the pons and medulla (when the pain/temperature fibers of the face are ipsilateral and the fibers of the body are contralateral). Imaging this level of a patient with this characteristic pattern of sensory loss will likely be informative.
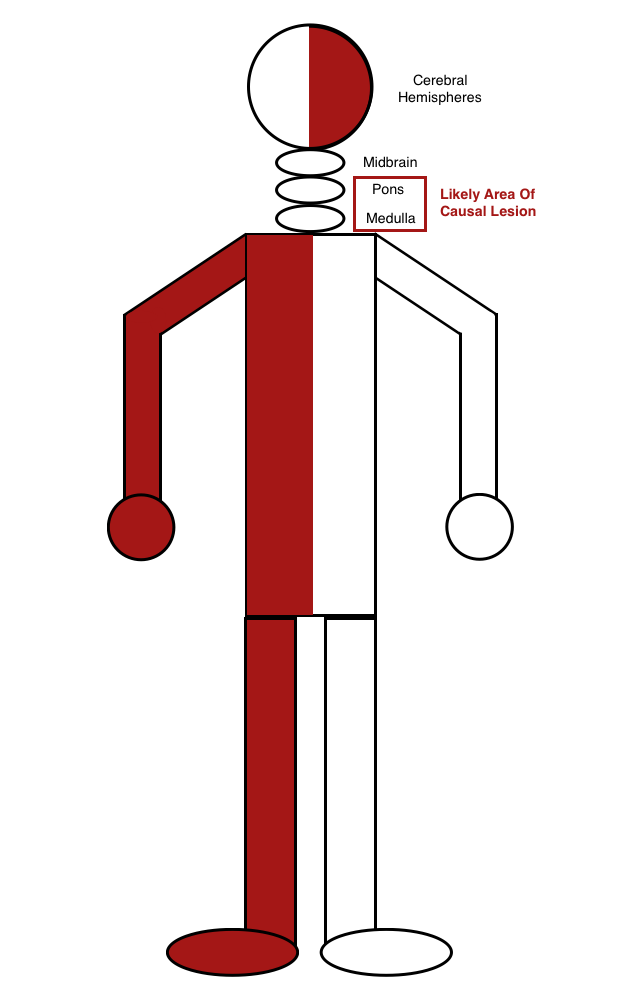
Motor weakness of the face, arm, and leg unilaterally can suggest the likelihood of a single casual lesion in the CNS system (because of how these neural pathways travel). The internal capsule of the brain can be a suspect area of interest.
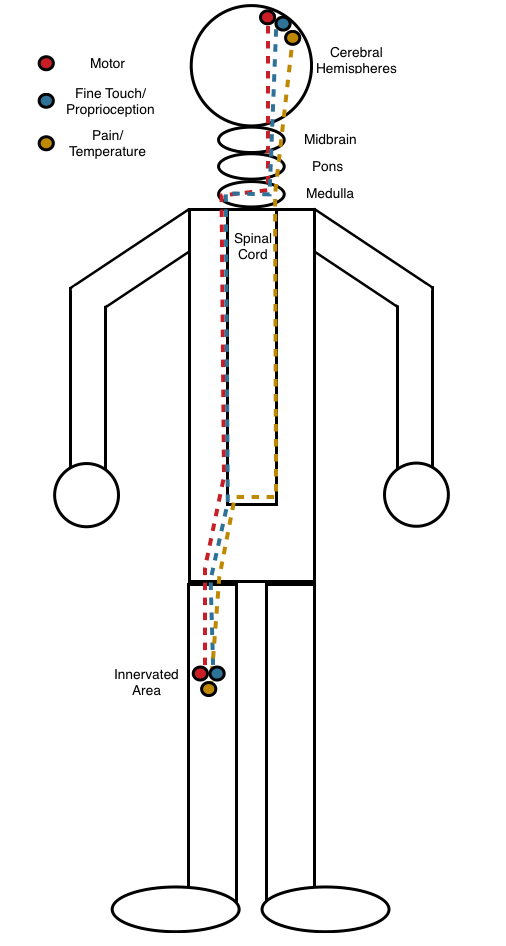
Loss of all pathways (motor and both sensory) unilaterally: if an area of the body has deficits in all of the pathways only on one side of the body, then it is very unlikely that that the casual leisoin resides in the spinal cord. This is because (within the spinal cord) the pain/temperature pathway runs contralateral to the innervated area, while both the motor and light touch/proprioception pathways run ipsilateral. If all three pathways were deficient in a patient unilaterally, in order for a lesion to reside in the spinal cord it would have to involve both sides of the spinal cord (unlikely). Similarly loss of pain and temperature with either the motor pathway or the light touch/proprioception pathway (deficits in only 2 pathways) also will likely exclude the spinal cord for similar reasons. Look to either the periphery or above the spinal cord in the CNS for such presentations.
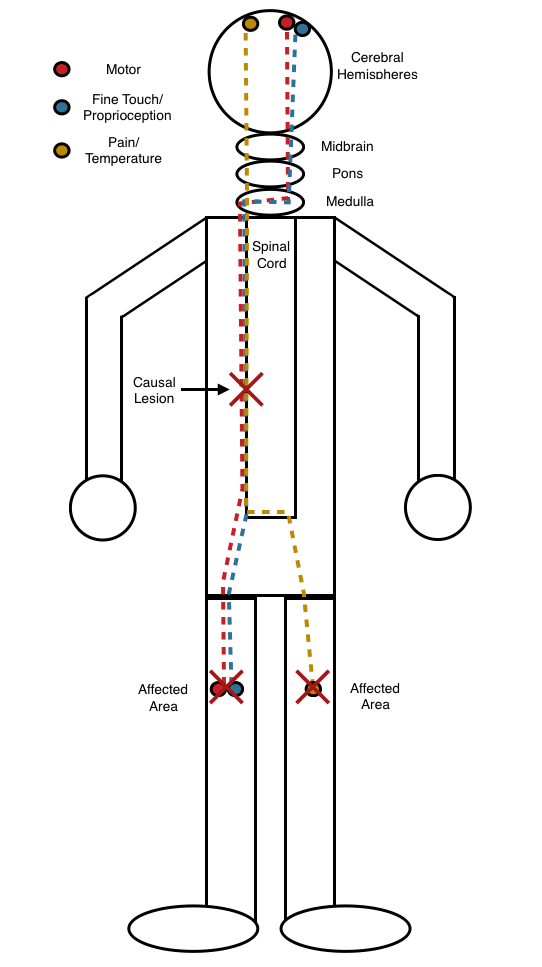
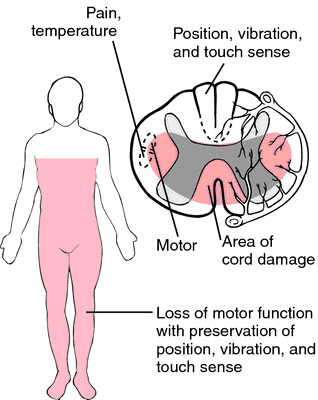
Different findings on opposite sides of the body: if pain and temperature is lost on one side, and either motor, fine touch/proprioception, or both are lost on the other side, then the causal lesion very likely resides in the spinal cord. This is because pan and temperature pathways travel on the contralateral side within the spinal cord, and the other two pathways are ipsilateral. The spinal cord is essentially the only location where such findings can be seen on opposite sides of the body.
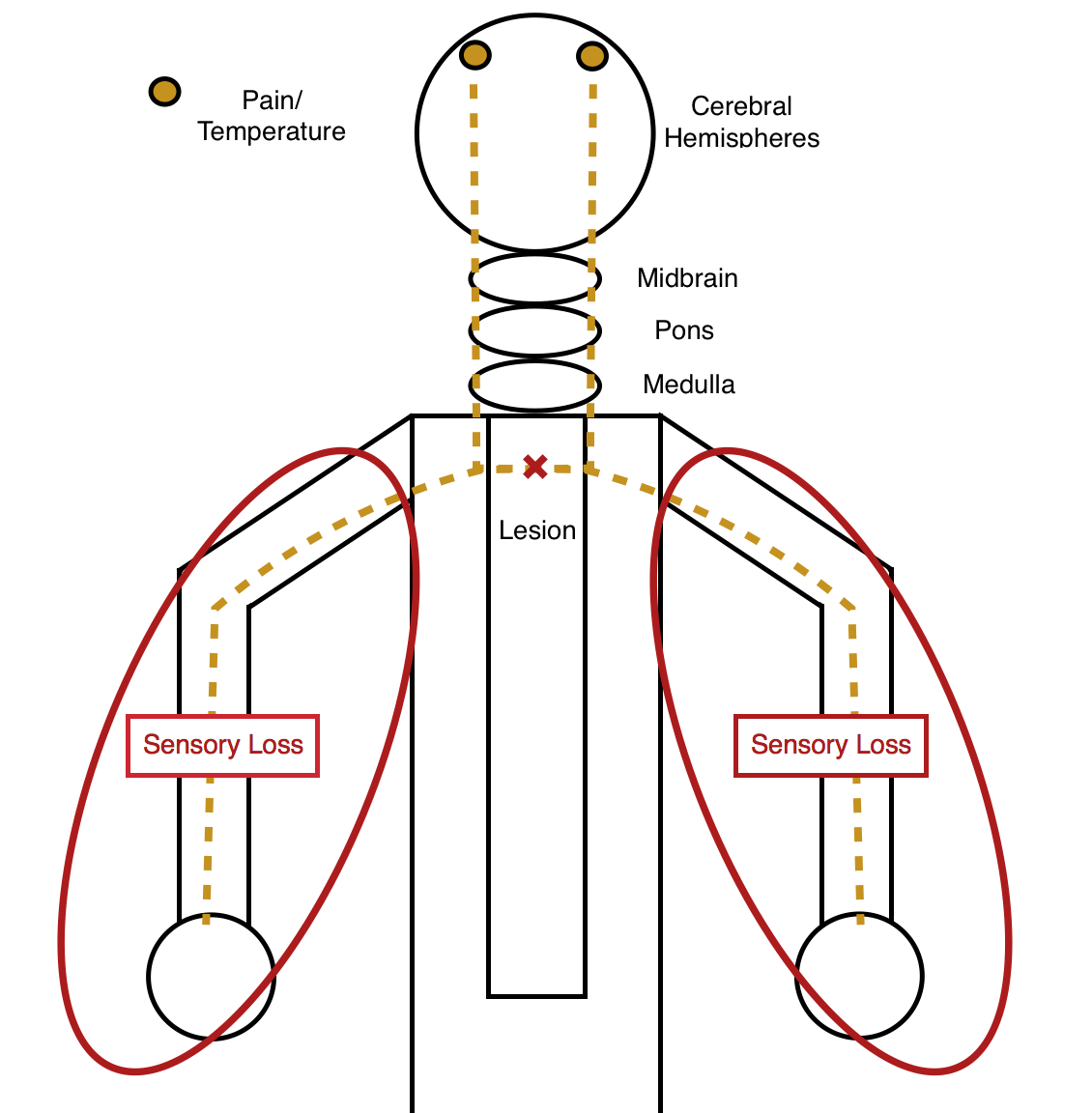
Bilateral symmetrical sensory (pain/temperature) loss: especially if this loss is only at one level of the body, can be very suggestive of a central cord lesion. This is because only the pain/temperature pathway will cross over to the other side of the body in the spinal cord, so a central lesion (in the ventral commissure) will selectively affect this sensation pathway (bilaterally) ONLY at the level of the lesion.
Bilateral motor and pain/temperature loss (intact light touch/proprioception): the anatomy of the spinal cord is such that the anterior spinal artery supplies everything except the light touch/proprioception pathway with blood. If there is an issue with the anterior spinal (such as an occlusion), the patient will lose motor and pain/temperature sensation bilaterally below the level of the issue (while keeping the other sensory pathway intact). This is called anterior cord syndrome.
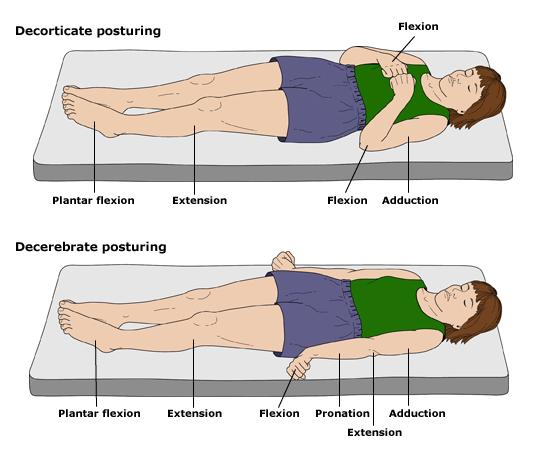
Decorticate vs. decerebrate posture: the red nucleus is found in the midbrain, and it is responsible for controlling flexor tone. As a result, damage above or below the red uncles can give these findings:
- Decorticate posture: increased flexor tone due to an intact red nucleus, combined with an issue upstream (damage to the cerebral hemispheres, the internal capsule, thalamus, or midbrain)
- Decerebrate posture: increased extensor tone due to a non-intact red nucleus. Damage in the brain stem below the red nucleus is the likely cause.
PNS: WHERE IN THE PERIPHERAL NERVOUS SYSTEM CAN THE ISSUE BE?
If the issue is peripheral we must decide where in the peripheral system it resides:
- Muscular
- Neuromuscular junction (NMJ)
- Peripheral nerve (either sensory/motor/both)
- Spinal root
Loss of only motor or sensory function: if only one pathway is affected in the patient, then it is very unlikely the diagnosis is a peripheral demyelinating disease (Guillain-Barré syndrome and chronic inflammatory demyelinating polyneuropathy/CIPD are examples). The reason for this is because peripheral nerves (both types of sensory and motor) travel together in bundles ensheathed in the same myelin. Should there be a demyelinating disease present, it would be very likely that it would selectively affect only motor or sensory pathways.
Sensory loss: if a patient presents with sensory loss than the issue is not primarily of the muscles or NMJ (because these are not responsible for sensation)
Diminished/absent reflexes: if a patient has diminished or absent reflexes then the issue very likely is not in the muscles or the NMJ, because only VERY severe impairment of these components will lead to noticeable differences on physical exam.
Present reflexes: if reflexes are present (and normal) then the sensory pathway leading to the spinal cord, as well as the motor pathway leading back to the muscle must be intact. Present reflexes do not rule out the possibility of a muscle or NMJ issue (see directly above for explanation)
PNS: DO KEY SPINAL ROOTS SEEM INVOLVED?
The following spinal root functions can potentially help localize peripheral nerve issues
- C3,4,and5keep diaphragm alive!
- C5 – Deltoid
- C6 – Biceps
- C7 – Triceps
- C8 -T2 Fingers
- L4 – Quadriceps
- L5 – Foot Dorsiflexion
- S1 – Plantar Flexion
- S2 – 5 Sphincter Control
ACKNOWLEDGMENTS
A very special thanks to Dr. Bernard Chang for making this page possible with his expertise.
Page Updated: 02.21.2016