Page Contents
OVERVIEW
This page is dedicated to organizing various examples of standardized exam questions whose answer is alpha-1 antitrypsin deficiency. While this may seem a odd practice, it is useful to see multiple examples of how alpha-1 antitrypsin deficiency will be characterized on standardized exams (namely the boards and the shelf exams). This page is not meant to be used as a traditional question bank (as all of the answers will be the same), however seeing the classic “test” characterization for a disease is quite valuable.
KEY CHARACTERISTICS OF THIS CONDITION (ON EXAMS)
When it comes to standardized exams, each condition has its own “code” marked by key buzzwords, lab findings, clues, etc. If you are well versed in this code you will be able to more quickly identify the condition that is being discussed, and get the right answer on the exam you are taking. Below is the “code” for alpha-1 antitrypsin deficiency.
Chief Complaints:
- Progressive/worsening shortness of breath is often the initial complaint.
Patient History:
- Young age: the patients typically will be younger then is expected for COPD
- No/limited past history of smoking is a red flag that something else might explain underlying etiology of patient’s respiratory condition.
- Family history of COPD (or lung disease) especially in young relatives can signify the presence of a genetic condition.
- Family history of liver cirrhosis (or liver disease) especially in younger relatives
Clinical Workup
- Prolonged expiratory phase which is consistent with obstructive lung conditions
- Crackles/rhonci/wheezes might be heard bilaterally
- Hyperinflation of lungs: can be reflected by decreased breath sounds, or seen on X-ray
- Increased lucency on X-ray especially at the bases. Air trapping in bases.
- Pulmonary function testing (often will diagnose COPD): redued FEV1 and FVC are common findings.
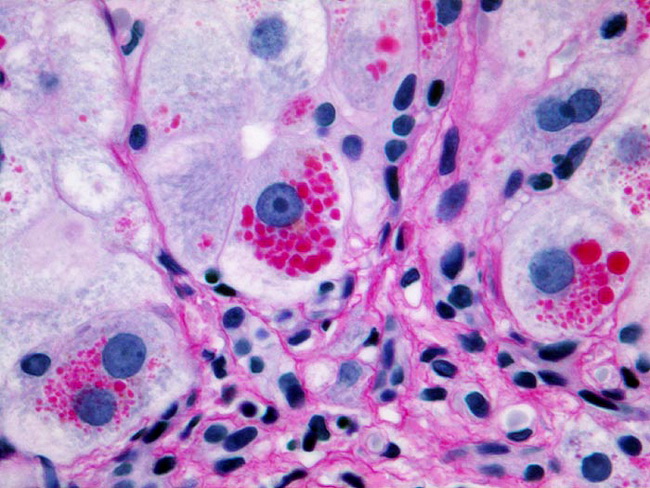
- Liver biopsy periodic acid-Schiff stain (PAS stain/histology): intracellular granules of unsecreated AAT can be seen in periportal hepatocytes of affected invidivudals. These granules will be reddish-pink with the PAS stain (PAS positive).
QUESTION EXAMPLES
Question # 1
A 40 year old male comes to his PCP because he has been experiencing worsening shortness of breath for the past 4 weeks. The patient has no past history of smoking or using tobacco products. He explains that his younger brother underwent a single lung transplant for severe COPD about 2 years ago. The patient’s respirations are 25/min and he is currently on supplemental oxygen. A physical exam reveals decreased breath sounds, and bilateral basilar crackles. A chest X-ray is ordered and increased lucency in the lung fields (especially at the bases) and flattened diaphragms. What is the likely cause of this patient’s symptoms?
Explanation # 1
Young age + progressive shortness of breath + no past history of smoking + family history of COPD (in young relative) + hyper-inflated lungs (increased lucency/flattened diaphragms) = alpha-1 antitrypsin deficiency
Question # 2
A 38 year old male comes to the physician because he has been noticing progressive shortness of breath for the past 6 months. He explains that he now has shortness of breath when he walks from his house to the mailbox. He normally is very active, however now is no longer able to exercise or go jogging with his friends. He does not smoke, and denies drinking alcohol. His family history is notable for a father who died of alcoholic cirrhosis at the age of 53. Currently his respiration rate is 22/min, and his oxygen saturation is 90% on room air. A physical exam reveals the presence of wheezes and rhonci bilaterally. A chest X-ray is ordered and reveals the presence of increased lung lucency at the lung bases. What condition is this patient most likely suffering from?
Explanation # 2
Young age + progressive shortness of breath + no past history of smoking + family history of liver cirrhosis (in young relative) + hyper-inflated lungs (increased lucency at bases) = alpha-1 antitrypsin deficiency
Question # 3
A 44 year old man comes to the clinic with yellowing skin and shortness of breath. He explains that he had a brief case of neonatal jaundice that resolved quickly, and he has not had any other episodes of it until now. The rest of his past medical history is unremarkable. He drinks very infrequently, and does not use tobacco products. A physical exam reveals scattered bilateral wheezes and decreased breath sounds. Lab results are shown below:
- Platelets: 135,000/mm³
- Total bilirubin: 4.2 mg/dL
- ALT: 95 U/L
The patient is tested for viral hepatitis infection, however the results are negative. A chest X-ray reveals the presence of hyperlucent lungs and flattened diaphragms. An abodminal ultrasound shows an increased liver span, and the liver parenchyma demonstrates increased echogenecity (however no masses are seen in the liver). What is the most likely diagnosis in this patient?
Explanation #3
Young patient + progressive shortness of breath + jaundice + signs of COPD (physical exam + X-ray) + likely liver cirrhosis (abdominal ultrasound results) = alpha-1 antitrypsin deficiency
Question # 4
A 45 year old man comes to the clinic because he has been experiencing progressive shortness of breath for the past several months. The patient denies any fever, weight loss, or cough. He has never smoked and does not use alcohol. Currently all of his vital signs are within normal limits. A physical exam reveals bilateral wheezes during respiration. Labs are ordered and the results are shown below:
- Platelets: 155,000/mm³
- WBC: 6,700/mm³
- Creatinine: 0.7 mg/dL
- Total bilirubin: 1.2 U/L
- ALT: 120 U/L
- AST: 110 U/L
A liver biopsy is performed to further reevaluate this patient. A periodic acid-Schiff stain is shown below
Given these findings, what likely explains this patient’s shortness of breath?
Explanation #4
Young patient + progressive shortness of breath + positive PAS stain (red granules seen on biopsy) = alpha-1 antitrypsin deficiency
Question # 5
A 36 year old male comes to the clinic because he has been suffering from progressive shortness of breath. He is normally very active however has been noticing that for the past year he slowly has been getting out of breath with shorter and shorter runs. He no longer is able to walk briskly without becoming short of breath. He comments that he has also begun to wheeze more recently. His past medical history is unremarkable, other then his recent attempt to take antihistamines to relieve his symptoms (which were unsuccessful). The patient admits to a 2 pack year history of smoking but has not smoked for the past decade. His family history is notable for his father who died from complications of both lung and liver disease at the age of 45. Pulmonary function testing shows a reduced FEV1 and a reduced FVC. What condition does this patient likely have?
Explanation #5
Young age + progressive shortness of breath + limited history of smoking + family history of lung/liver disease (in young relative) + pulmonary function testing indicative of COPD = alpha-1 antitrypsin deficiency
Question # 6
A 45 year old male comes to the physician because he has been experiencing worsening shortness of breath. He has no past history of smoking tobacco products but admits to trying marijuana a few times back in college. A physical exam reveal diffuse wheezing across both lung fields, and palpation of the abdomen suggests the presence of hepatomegaly. Pulmonary function tests are conducted and show a decreased FEV1 and FRC. A chest X-ray is ordered and demonstrates hyperinflation of both lungs, with air trapping at the bases. What is the likely diagnosis in this patient?
Explanation #6
Young age + progressive shortness of breath + limited history of smoking + pulmonary function testing indicative of COPD + hyperinflation of lungs on X-ray = alpha-1 antitrypsin deficiency
COMMONLY ASKED QUESTIONS ABOUT THIS CONDITION (BEYOND ITS IDENTIFICATION)
Many questions on standardized exams go beyond simply recognizing the underlying condition. Often there are specific testable questions regarding some aspect of the diseases pathophysiology/management/clincial implications that are commonly asked. Some of these are listed below:
Cause:
- Base issue: deficiency of alpha-1 antitrypsin (AAT)
- Inheritance: autosomal, codominant
- What is AAT: this enzyme is a serum protein that inhibits several different protelyitc enzymes (including neutrophil elastase). The net effect is that it stops the destruction of proteins such as elastase.
- Consequence of AAT deficiency: destruction of proteins (such as elastase) in the liver and the lungs.
- What does it cause in the lungs: panacinar emphysema due to the unchecked destruction of alveolar walls.
Diagnostic Testing:
- Serum AAT levels can be measured
- Confirmatory genetic testing can be done as well (to find causal mutation)
Page Updated: 04.01.2017