Page Contents
- 1 OVERVIEW
- 2 WHAT IS HYPONATREMIA?
- 3 WHY IS IT A PROBLEM?
- 4 WHAT MAKES US SUSPECT HYPONATREMIA?
- 5 HOW IS HYPONATREMIA DIAGNOSED?
- 6 DETERMINING SERUM/URINE OSMOLALITY
- 7 HYPERTONIC HYPONATREMIA
- 8 ISOTONIC HYPONATREMIA
- 9 HYPOTONIC HYPONATREMIA: THE IMPORTANCE OF VOLUME STATUS
- 10 HYPOTONIC HYPONATREMIA: VOLUME OVERLOAD STATE
- 11 HYPOTONIC HYPONATREMIA: EUVOLEMIC STATE
- 12 HYPOTONIC HYPONATREMIA: VOLUME DEPLETED STATE
OVERVIEW
This page is dedicated to building a framework for how to approach hyponatremia. This seemingly simple electrolyte disturbance requires a very systematic and intentional workup that is characterized below.
WHAT IS HYPONATREMIA?
Quite simply, hyponatremia refers to low levels of sodium within the serum. It is defined by sodium levels that are <135 mmol/L (although reference ranges may vary depending upon the lab doing the assay).

WHY IS IT A PROBLEM?
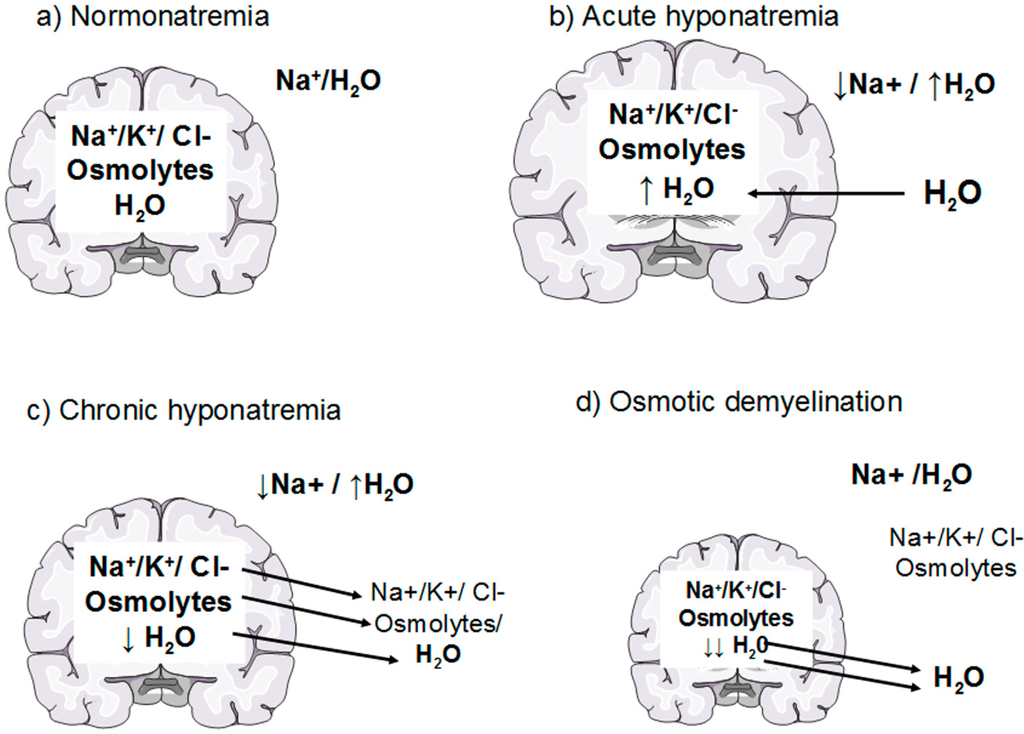
Sodium is an important electrolyte for the function of many different cells and tissues within the body. It is for this reason that a specific concentration of sodium is maintained within the serum. In the setting of hyponatremia, water will be osmotically driven into the brain cells in order to maintain this serum concentration. This in turn will result in cerebral edema and increased intracranial pressure. This can be dangerous (leading to deadly processes such as brain herniation) and also will cause the neurological symptoms elaborated more below.
WHAT MAKES US SUSPECT HYPONATREMIA?
Risk factors
Excessive water intake, diuretic usage, congestive heart failure, portal hypertension
Presenting symptoms/chief complaints: severity depends on the extent of hyponatremia.
Mild hyponatremia may include symptoms of:
- Nausea
- Malaise
Moderate hyponatremia (often a chronic process) can present with:
- Headache
- Lethargy
- Restlessness
- Weakness
- Disorientatoin
Severe/rapid onset of hyponatremia can result in:
- Seizures
- Coma
- Respiratory arrest
Physical exam
Volume status (while by itself not used to suspect hyponatremia) is often very important to assess when working up hyponatremia. This determination of volume status ideally occurs when the patient is first met, however after confirmed hyponatremia it is worth verifying.
- Volume overload will be evident in the setting of edema (peripheral, periorbital, ascites, elevated JVP, pulmonary edema/lung crackles)
- Volume depletion can be suggested if the patient has dry mucous membranes, skin tenting, and/or hypotension.
- Euvolemia is the absence of any clinical signs of volume overload/depletion (i.e. no edema, moist mucous membranes, no skin tenting).
HOW IS HYPONATREMIA DIAGNOSED?
The formal diagnosis of hyponatremia is made from measuring serum sodium (from a test such as a basic metabolic profile). Once this diagnosis is made, we need to have a methodology for discovering what is causing hyponatremia in our patient.
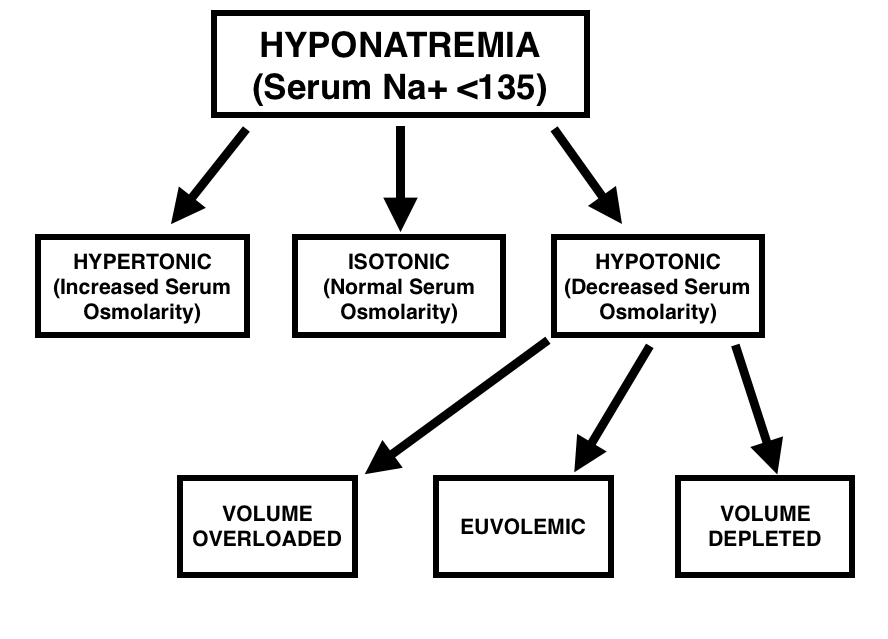
It is important to realize that while hyponatremia can be diagnosed from the serum value, its cause can not. Because the differential for hyponatremia is very broad, we must break it down into categories that each have their own clinical workup. A broad overview of this is shown in the figure below.
DETERMINING SERUM/URINE OSMOLALITY
The initial characterization of hyponatremia benefits from evaluating serum osmolarity: this will help us determine (in part) what type of hyponatremia we are dealing with. This value can be calculated from serum electrolyte values (reported from tests like the basic metabolic panel) using the online calculator here. The tonicity of the hyponatremia is classified in the categories below (each with their own subset of differential diagnosis)
- Hypertonic hyponatremia generally considered in patients with an osmolality above 295 mosm/L
- Isotonic hyponatremia will often have serum osmolality values in the 285-295 mosm/L range.
- Hypotonic hyponatremia (and its causes) should be explored in patients who have serum osmolality values below 295 mosm/L.
**It is important to appreciate that having HARD cutoffs for these categorizations is not advantageous. Patients with borderline values should be considered for various causes of hyponatremia that span both tonicity categories**
Let us take note that urine studies are important to order early on: while these values will be used later in our diagnostic path (utility of urine values explained more below) it is important that chronologically we order the following studies early on in our workup.
- Urine osmolality: this value will give us a sense of how concentrated or dilute the urine is holistically.
- Urine sodium (urine spot sodium): calculating the current concentration of sodium in the urine can be useful later on.

HYPERTONIC HYPONATREMIA
This is often referred to as pseudohyponatremia because while patients do have low serum concentrations of sodium, the real issue revolves around the excessive osmotic pressure in the patients blood that draws water from other compartments, and dilutes what initially was a normal serum sodium.
Hyperglycemia is often the cause of this particular type of hyponatremia. Excessive osmoles (in this case glucose) will draw water from other compartments and lower the serum sodium values. The glucose value from the basic metabolic panel used to diagnose the hyponatremia can help provide context on this presentation.

Hypertonic infusion (glucose, mannitol): while a different source of osmoles compared to traditional hyperglycemia, the IV administration of hypertonic solutions (such as glucose) can cause a similar phenomenon of hypertonic hyponatremia.
ISOTONIC HYPONATREMIA
This type of hyponatremia is generally a lab error: this issue generally affected older methods of calculating serum sodium (although this issue may persist depending on the care setting). Essentially, some modalities for testing will take the aqueous layer from centrifuged blood and use the entire volume of the sample to estimate the serum concentration of sodium. Normally this is not an issue, however in the setting of elevated serum proteins/proteins this will become misleading. This is because a significant portion of the blood will actually contain these proteins/lipids (components that will not contribute sodium to the aqueous layer). As a result, the net calculated sodium is divided by the total volume (even though much of that volume was actually protein/lipids) artificially decreasing the reported serum sodium value.

HYPOTONIC HYPONATREMIA: THE IMPORTANCE OF VOLUME STATUS
Hypotonic hyponatremia is the most provocative of our categories discussed, simply because this is where the bulk of causes of hyponatremia lie. Going back to our physical exam, we must now rely upon volume status of the patient to help further tailor our clinical workup to the exact type of hyponatremia we are dealing with. Each category of volume status has its own separate differential diagnosis and workup that
- Volume overloaded hyponatremia will present with edema/ascites on exam.
- Euvolemic hyponatremia will not show any signs of volume overload/depletion.
- Volume depleted hyponatremia will present with signs of dry mucous membranes, skin tenting, and sometimes hypotension.
HYPOTONIC HYPONATREMIA: VOLUME OVERLOAD STATE
In the setting of volume overload excess volume has left the vascular compartment and has collected elsewhere. It is for this reason that this type of hyponatremia will present with edema and ascites. The cause of the volume shift will be specific to the underlying disease process.

One of our initial steps in working up this type of hyponatremia is to take a look at the urine spot concentration of sodium. It is important to keep in mind that there are no true hard cutoffs with this lab value, however the values used below are useful for organizing the differential.
If the urine sodium is low ( < 20-30 mmol/L) this will suggest that sodium is not lost by renal excretion, and the edematous state is more likely responsible for the perceived hyponatremia. Diseases processes to consider are:
- Congestive heart failure: pulmoanry and peripheral edema may be responsible here
- Liver cirrhosis/portal hypertension: ascities fluid in the abdomen can be a contributor
- Nephrotic syndrome: can have periorbital or peripheral edema
If the urine sodium is high (>20-30 mmol/L) the source of sodium loss is very likely the kidney (this value suggests poor re-absorption in the setting of hyponatremia). Possibilities include.
- Renal failure: intrinsic defect/damage to the kidney rendering it unable to re-absorb sodium
- Diuretic usage: iatrogenic causes of increased sodium wasting by the kidney.
HYPOTONIC HYPONATREMIA: EUVOLEMIC STATE
In the setting of euvolemia we must appreciate the general idea of what is going on. Patients in this setting are re-absorbing too much water (the absence of re-absorbing sodium). A few conditions can be responsible for this type of presentation, and below is an organized methodology for working up this particular type of hyponatremia.
Important diagnosis to evaluate in all patients: while there may be exceptions, in the setting of hypotonic hyponatremia with a euvolemic state, it is important to make sure that the patient does not have the following conditions:
- Hypothyroidism: checking a recent TSH (or sending off a new thyroid study) should be one of the first thoughts here. Hypothyroidism can cause hyponatremia by increasing water retention (diluteinal hyponatremia).
- Adrenal insufficiency (mostly primary but sometimes secondary): is important to investigate as a possibility as well (basal cortisol levels and ACTH levels can be useful). Fundamentally the loss of aldosterone/mineralcorticoid activity will impair the kidney’s ability to re-absorb sodium.
Utility of urine osmolality: while evaluating for the above endocrine reasons for hyponatremia we can also help organize our differential by the relative concentration of the urine.
If the urine osmolality is high (> 100 mOsm/kg) then we must consider disease processes that would be characterized by inappropriate water movement from the urinary filtrate, back into the body. This is generally going to be the result of SIADH which has the following major causes:
- Ectopic ADH secretion/paraneoplastic: this can be due to small cell lung carcinoma or a intracranial neoplasm
- CNS disorders/ head trauma: can lead to increased ADH secretion by the pituitary
- Pulmonary disease/infection: can be secondary to pneumocystis infection (in AIDS patients)
- Drug reactions: Carbamazepine, Cyclophosphamide, SSRI
- Mutations: in the V2 receptor for ADH can lead to increased ADH signaling even in its absence.
If the urine osmolality is low (> 100 mOsm/kg) we must now consider scenarios where too much free water has been introduced into the body. Possibilities include:
- Psychogenic polydipsia: patients with excessive oral water intake are able to cause hyponatremia.
- Excessive administration of IV hypotonic fluids: it is important to keep in mind that this type of hyponatremia can be caused iatrogenically.
HYPOTONIC HYPONATREMIA: VOLUME DEPLETED STATE
Volume depletion requires a route of volume loss paired with the ingestion of water. Sodium containing fluids are lost and replaced with free water (which leads to hyponatremia!). Our first step here will be to look at urine sodium values to help narrow our differential.
If the urine sodium is low ( < 20-30 mmol/L) this will suggest that sodium is not lost by renal excretion. Possible causes can include:
- Dermal losses such as sweating or burns
- GI losses such as vomiting, diarrhea
- Fluid sequestration by diseases such as pancreatitis
- Blood loss that is is severe enough to lower patient’s volume status
If the urine sodium is high (>20-30 mmol/L) the source of sodium loss is very likely the kidney (this value suggests poor re-absorption in the setting of hyponatremia). Possible causes can include:
- Diuretics
- Salt-wasting nephropathy
- Cerebral salt wasting
- Mineralocorticoid deficiency caused by diseases such as adrenal insufficiency
Page Updated: 07.26.2016