Page Contents
- 1 Overview
- 2 CN I (Olfactory Nerve)
- 3 CN II (Optic Nerve)
- 4 CN III (Oculomotor Nerve)
- 5 CN IV (Trochlear Nerve)
- 6 CN V-1 (Trigeminal nerve ophthalmic branch)
- 7 CN V-2 (Trigeminal nerve maxillary branch)
- 8 CN V-3 (Trigeminal nerve mandibular branch)
- 9 CN VI (Abducens nerve)
- 10 CN VII (Facial nerve)
- 11 CN VIII (Vestibulocochlear nerve)
- 12 CN IX (Glossopharyngeal nerve)
- 13 CN X (Vagus nerve)
- 14 CN XI (Accessory nerve)
- 15 CN XII (Hypoglossal nerve)
- 16 Cranial Nerve Skull Exits – Localization
Overview
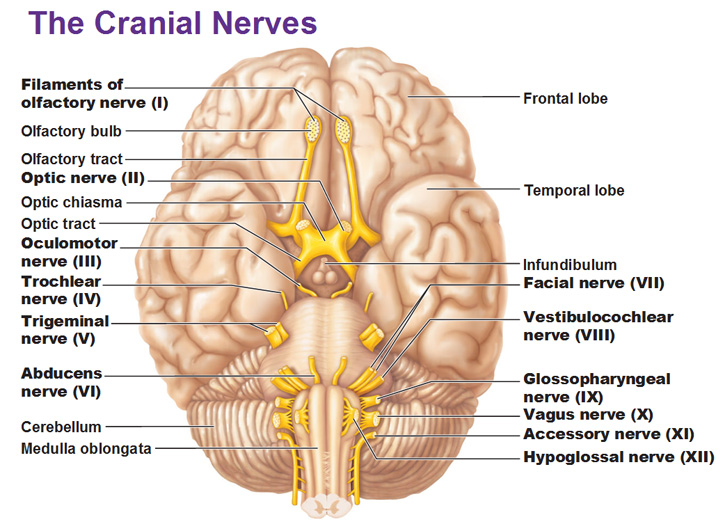
Below are the general locations of the cranial nerves on gross examination.
CN I (Olfactory Nerve)
Exit: Cribriform plate
Function: afferent olfactory (nerve only travels from sinus to bulb; olfactory tract is what you see on the brain from bulb to olfactory cortex)
Clinical Facts: Parkinson disease can often present with loss of smell before anything else
HOW TO TEST: Generally it is acceptable to ask the patient about their sense of smell (and if it has changed) instead of directly testing this nerve. In order to test the nerve have the patient close their eyes (and one nostril, make sure to test each nostril independently), place soap/disinfectant (found in all patient rooms) in your hand, and ask patient if they can smell anything/what they smell when you place it close to their nose.
CN II (Optic Nerve)
Exit: Optic canal
Function: afferent visual from retina (not a nerve at all, but an extension of the brain)
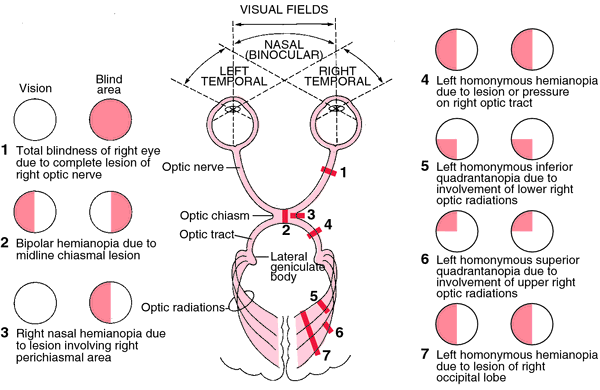
Clinical: loss of vision/visual acuity in the eye is suggestive of problems with this nerve
HOW TO TEST:
Visual acuity: to test visual acuity one can use a snell card. Make sure to test each eye individually!
Visual fields: testing each eye individually, check the 4 quadrants/visual fields deliberately (see image below). Facing the patient, have them close one eye and close your opposite eye as well (if the patient closes their right eye, you will close your left in order to replicate normal monocular visual fields for the exam). Have the patient focus on your nose and ask them if any part of your face is blurry/seems missing.
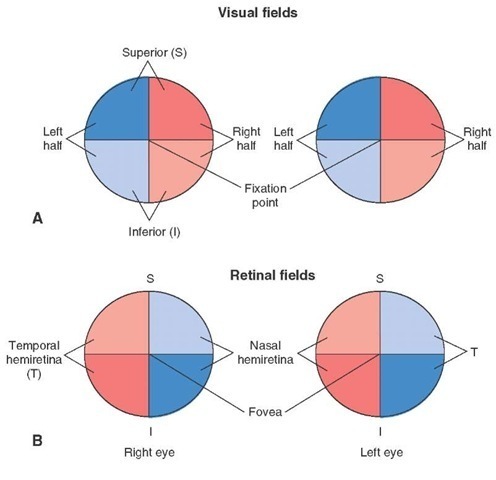
Without the patient moving their eye (keeping focus on your nose) move your hand (keeping it equidistant between you and the patient) into each quadrant and assess the integrity of the visual field (can hold up fingers and have the patient tell you how many, or can have the patient tell you when your fingers start wiggling). Repeat the test with the other eye.
Pupillary reaction to light: follow the order of events below and you will get the most out of this exam:
- Shine penlight into one eye and observe the same eye for constriction.
- Shine penlight into the same eye again, and observe opposite eye for constriction.
- Repeat steps 1-2 for the other eye.
- Conduct swinging flashlight test, second eye should constrict slightly after flashlight moves to the other eye (direct stimulation of light is stronger than contralateral constriction compensation). Eye should most definitely NOT dilate
- Repeat step 5 for the other eye.
CN III (Oculomotor Nerve)
Exit: superior orbital fissure
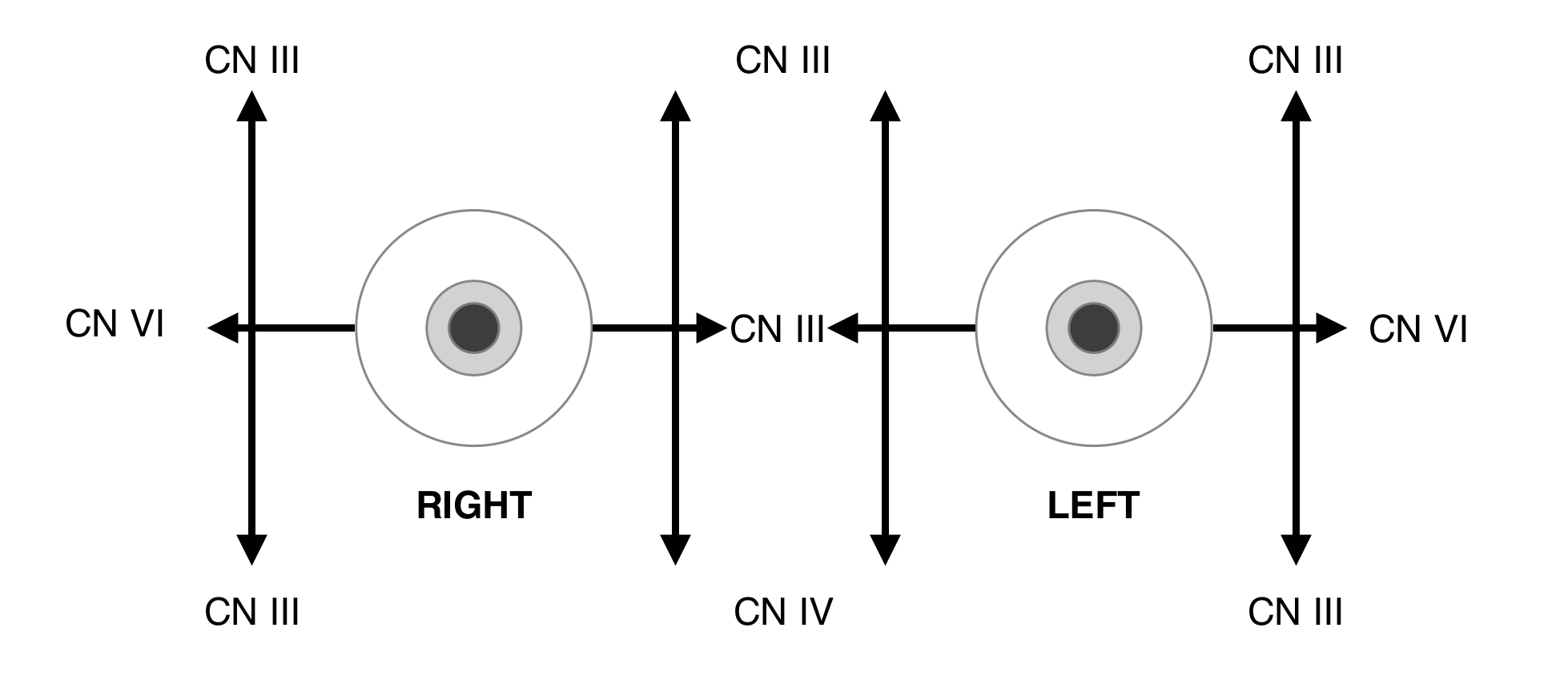
Function: efferent motor to eye (medial, superior, and inferior rectus muscles and inferior oblique muscle, levator palpebrae); efferent parasympathetic to eye (pupillary constriction)
Clinical:
Ptosis: eye drooping due to lack of levator palpebrae function. In the image below the patient has potties of the left eye (an issue exists with the left oculomotor nerve).

Loss of eye movements: most of the eye movements are controlled by this nerve. When checking ocular movements (excluding adducted depression and abduction) any issue with the other movements is controlled by this nerve.
Issues of pupillary constriction: It is important to keep in mind that tonically dilated pupils are also possible due to CN III nerve partial palsy.
**Horner syndrome (seen below in the left eye) is a loss sympathetic activity which causes miosis, a tonically constricted eye (which is controlled parasympathetically), and ptosis (also seen below in the left eye). This is not an issue with the CN III but can fool some physicians with regards to its initial clinical presentation. The ptosis is caused by loss of activity of the superior tarsal muscle. Anhidrosis (decrease sweating) is also present. The site of the lesion is ipsilateral to the ptosis, mitosis, and anhidrosis.

HOW TO TEST:
Observe the patient for any ptosis or pupillary constriction issues. Have the patient focus on either your finger or a pen, and move it in a “H” pattern (see below). Take note of any issues with ocular movement.
CN IV (Trochlear Nerve)
Exit: superior orbital fissure
Function: efferent motor to superior oblique muscle (depresses the eye when adducted in isolation)
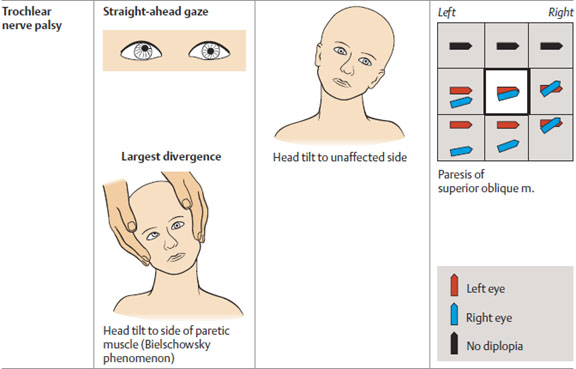
Clinical: Inability to depress the eye when adducted. In acquired lesions of fourth nerve, patients report vertical, torsional, or oblique diplopia. Diplopia is usually worse on downgaze and gaze away from side of affected muscle. **Patients often adopt a characteristic head tilt, away from affected side to reduce their diplopia.
CN V-1 (Trigeminal nerve ophthalmic branch)
Exit: superior orbital fissure
Function: afferent sensory from upper face, including cornea (forehead, upper eyelid, cornea, conjunctiva, dorsum of nose, nasal membranes)
Clinical: This branch of the nerve mediates the corneal reflex (involuntary blinking of the eyelids elicited by stimulation of the cornea). *Only carries sensory information!
HOW TO TEST:
Using a broken cotton swab touch the patients fore head bilaterally to assess for intact sensation (one side can test pinprick, the other fine touch).
Corneal reflex can be tested with the end of a cotton ball.
CN V-2 (Trigeminal nerve maxillary branch)
Exit: foramen rotundum
Function: afferent sensory from middle portion of face and upper jaw (upper lip, lateral nose, upper cheek, anterior temple, membranes of nose, upper jaw and teeth, roof of mouth).
Clinical: *Only carries sensory information!
HOW TO TEST:
Using a broken cotton swab touch the patients fore head bilaterally to assess for intact sensation (one side can test pinprick, the other fine touch).
CN V-3 (Trigeminal nerve mandibular branch)
Exit: foramen ovale
Function: efferent motor to muscles of mastication; afferent sensory to lower face and jaw (lower lip, chin, posterior cheek, temple, external ear, lower jaw and teeth, cheeks, floor of mouth, anterior two thirds of tongue)
Clinical: loss of nerve function should affect muscles of mastication. Sensory innervation of anterior two thirds of the tongue (NOT TASTE!)
HOW TO TEST:
Using a broken cotton swab touch the patients fore head bilaterally to assess for intact sensation (one side can test pinprick, the other fine touch).
Masseter exam: have patient clench teeth and feel for muscle contraction in the face. Can also feel for clenching in temporal muscles.
CN VI (Abducens nerve)
HOW TO TEST:
On the “H” test for eye movement observe abduction of both eyes. The lateral rectus muscle (innervated by the abducens nerve) is responsible for this movement.

CN VII (Facial nerve)
Exit: internal auditory meatus
Function: efferent motor to superficial facial muscles and stapedius (also posterior belly of digastric muscle); efferent parasympathetic fibers (lacrimal and salivary glands); afferent gustatory (taste) from anterior tongue; afferent sensory from portion of external ear skin
Clinical:
- Loss of stapedius control => more vibratory tympanic membrane (less stabilized) => higher volumes registered. Patients will complain of loud noises.
- Upper facial movements (i.e. eyebrow raise) is controlled bilaterally. CNS/upper motor neuron issue on one side with this nerve will cause only lower facial motor issues (such as facial droop). CNS lesions can cause this, and it is more serious!
- Lower motor neuron issues will cause paralysis of the whole side of the face (upper and lower) because at this point both sides of the brain have come together to control the upper face. Lyme disease and herpes zoster in the peripheral nervous system can cause this and it manifests as something called Bell’s Palsy (image below, most right, shows palsy on the right side of the patients face).
HOW TO TEST:
Other than normal observations (no ptosis, face droop, etc) you should assess upper and lower portions of the face (given separate innervation). Ideally have the patient conduct the following 3 things to look for weakness/asymmetry:
- Have the patient raise eyebrows
- Have patient shut eyes very tightly
- Have patient show all of their teeth/smile

*Don’t confuse paralysis on one side for ptosis on the other!
CN VIII (Vestibulocochlear nerve)
Exit: internal auditory meatus
Function: afferent vestibular information from labyrinth; afferent auditory information from cochlea
Clinical: balance and hearing. Vertigo and hearing loss can occur when patients have an issue with this nerve. Patients fall toward the side they have the issue (i.e patients with left CN VIII lesions will fall to the left).
HOW TO TEST:
There are 3 major parts to this portion of the exam.
1.) Rubbing finger test: can the patient hear you rubbing thumb/fingers next to each ear? This is usually sufficient for a basic screening exam.
-One can whisper a number in one ear while they rub fingers in the other to see if patient can hear the number when distracted.
2.) Rinne test: strike 512 Hz tuning fork and hold base at mastoid bone. Follow these instructions below very carefully for both ears
– Ask patient if they can hear the fork when it is contact with the mastoid bone (they should be able to)
– Have the patient tell you the moment they no longer can hear the fork vibrating.
– As soon as this occurs hold the tines of the still vibrating fork next to the ear of the patient and ask if they can now again hear it. In a normal individual they should! The sound in the air medium should be louder than in the bone.
–If they can’t initially hear the fork, there is a sensory issue.
-If they can hear the fork initially, but it is not louder in the air medium, their is a conduction issue.
3.) Weber test: strike the 512 fork and hold base at the forehead. Ask patient where the sound is localizing. If the sound of the fork vibrating is equal in both ears, this is a normal result. If it localizes to one ear, their are two possibilities:
– The ear hearing more sound is abnormal and has a conduction issue (plugging a normal ear with a finger will replicate this phenomenon)
– The ear hearing less sound is abnormal and has a sensory issue.
CN IX (Glossopharyngeal nerve)
Exit: jugular foramen
Function: efferent motor to pharynx skeletal muscle; efferent parasympathetic fibers to parotid gland; afferent sensory from portion of external ear skin; afferent sensory from pharynx, middle ear, carotid body and sinus; afferent gustatory (taste) from posterior tongue.
Clinical: can check posterior tongue ability to taste. Overlap in muscle function with Vagus nerve.
HOW TO TEST:
See below for testing the vagus nerve (CNS IX and X tested together).
CN X (Vagus nerve)
Exit: jugular foramen
Function: efferent motor to striated muscle of palate, pharynx, larynx; efferent parasympathetic fibers to viscera; afferent sensory from portion of external ear skin, meninges; afferent sensory from larynx, trachea, gut, aortic arch; afferent taste from larynx
Clinical: difficulty swallowing, uvula deviation away from the side of the issue.
HOW TO TEST:
have the patient open their mouth and look back into the back of their throat. Have the patient swallow with their mouth open.
– Make sure the palate is able to be raised properly
– Check to make sure the uvula is and remains in the middle. The uvula will deviate away from the side of palate weakness (towards the strong/normal side)

CN XI (Accessory nerve)
Exit: jugular foramen
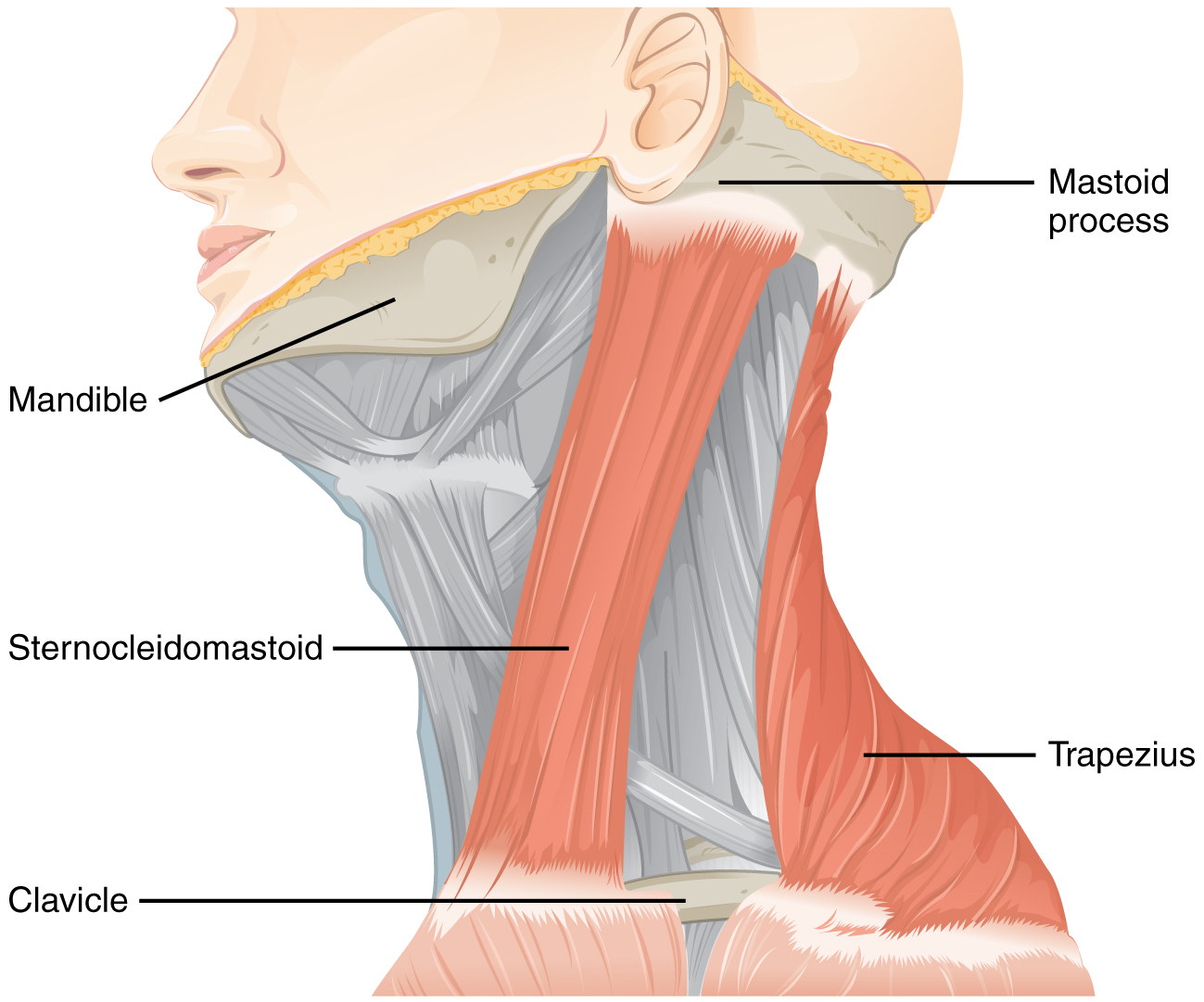
Function: efferent motor to sternocleidomastoid and trapezius
Clinical: issue on one side will impair neck turning towards the opposite side
HOW TO TEST:
Have the patient turn their neck turn to each side. Turning to one direction tests the function of the sternocleidomastoid muscle on the opposite side. Oppose this turning movement to check strength (can place a hand on the chin to provide resistance) .
Have the patient shrug their shoulders (both together and one at a time). This movement can also be opposed to check for strength.
CN XII (Hypoglossal nerve)
Exit: hypoglossal canal
Function: efferent motor to tongue (intrinsic and extrinsic)
Clinical: the tongue will deviate (when stuck out) to the side of weakness.
HOW TO TEST:
Have the patient stick out their tongue, and then move it side to side. The tongue will deviate toward the side of weakness/nerve damage. Muscle atrophy can also be visible on exam so symmetry can be assessed.
– Can also check strength if desired (and if there is time): have patient push out their cheek from the inside of their mouth and oppose their movements.

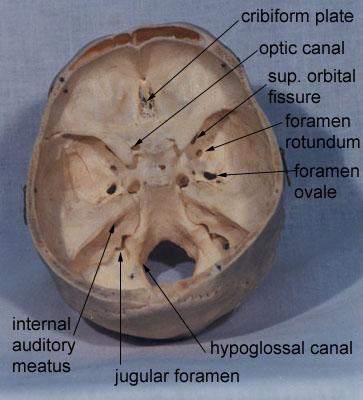
Cranial Nerve Skull Exits – Localization
***Issues with nerves in these constellations implicates the respective skull exit simply because this is where all of these nerves co-localize.
- Superior orbital fissure: CN III, IV, VI, and V-1 (ophthalmic division)
- Cavernous sinus: CN III, IV, VI, V-1 and V-2
- Internal auditory canal: CN VII, VIII
- Jugular foramen: CN IX, X, XI
*Other CN’s have individual foramen
Page updated: 01.01.2016