Page Contents
OVERVIEW
This guide is dedicated to helping establish a framework for working up a patient who complains of symptoms suggestive of urethritis. These include:
- Dysuria (which can also be described as burning during urination)
- Urethra discharge that can be watery to frankly purulent. It can be scant in presentation (and sometimes only is present on the first morning void)
- Penile/vaginal pruritus is a common presentation as well.
Urethritis is very suggestive of some type of sexually transmitted infection (that will be elaborated more below.
*It is important to appreciate that some patients will be asymptomatic even thought the possess an infective cause of urethritis.
INTIIAL CLASSIFICATION: GONOCOCCAL VS. NONGONOCOCCAL
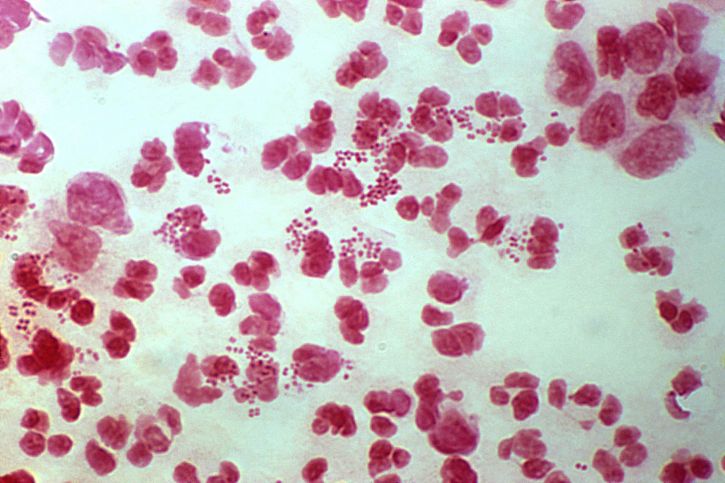
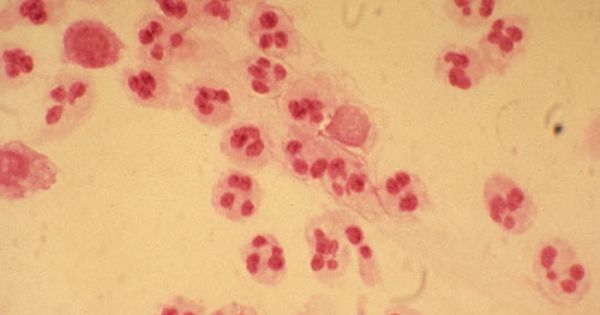
While urethral swabs are not as common as they once were, it is important to understand how they can be a very quick way to characterize the type of urethritis a patient may possess (as either gonococcal or nongonococcal (each with its own individual diagnostic path). This procedure is exactly as it sounds. A swab is used to capture the infectious organism in urethra, and is then gram stained/stained with methylene blue for visualization under light microscopy. This can be done quickly at the initial clinic visit so that following treatments and diagnostic evaluations can be tailored to 1 of 2 paths! This will save time and money!
Gonococcal urethritis: the utility of the urethral swab is that if the cause of the patients symptoms is a gonococcal infection, this can be visualized very quickly under the microscope. Intracellular/extracellular diplococci will be present in the urethral exudate (either gram negative or dark purple depending on stain used). From this point on the diagnostic path is much less vast.
Nongonococcal urethritis (NGU): if the gram stain only shows white blood cells and no pathogens that can be visualized with a gram stain, then a different diagnostic path must be taken.
CHARACTERIZING/TREATING GONOCOCCAL URETHRITIS
If microscopy demonstrates gonococcal urethritis, then almost certainly the cause of the patients symptoms is the bacteria Neisseria gonorrhoeae.
Confirmatory testing can invovle a nucleic acid amplification test (NAAT) for Neisseria gonorrhoeae on first voided urine however the gram stain results are likely enough to begin treatment.
Treatment involves a single intramuscular dose of ceftriaxone (250 mg) and a single dose of azithromycin (1 gram). This treatment also covers chlamydia.
CAUSES OF NONGONOCOCCAL URETHRITIS
If microscopy does not demonstrate gonococcal urethritis. Then the causal pathogen/process must be identified. The likely candidates include:
- Chlamydia trachomatis is the most likely and often empirically treated.
- Mycoplasma genitalium
- Ureaplasma urealyticum
- Trichomonas vaginalis
- Treponema pallidum
- Herpes simplex virus can be the cause of urethritis (however generally a clinical exam will reveal signs of genital herpes).
- Other unspecified pathogens might also be the cause of a patients urethritis (if all of the above have been ruled out). Many cases do not have a clear etiology. They have been associated with men who have sex with men and bacterial vaginosis (source)
Non STI causes of dysuria: should all of the pathogens/processes above be ruled out it is important to appreciate that the below infective processes might also present with dysuria.
- Cystitis
- Epididymitis
- Prostatitis
Noninfectious causes of urethritis: should all of the pathogens/processes above be ruled out, noninfectious causes of the patients symptoms should be explored:
- Chemical irritation: spermicides and soaps
- Stripping of urethra by the patient (trauma)
DIAGNOSING CAUSE OF NONGONOCOCCAL URETHRITIS
Generally the assumption is that NGU is caused by Chlamydia trachomatis and the patient s
NONINFECTIOUS CAUSES OF URETHRITIS
FURTHER READING
Page Updated: 06.07.2016