Page Contents
- 1 OVERVIEW
- 2 THE DIGITAL RECTAL EXAM (DRE)
- 3 CAUSES OF FALSELY ELVEATED PROSTATE SERUM ANTIGEN (PSA) LEVELS
- 4 WHY DO SOME RECOMMEND AGAINST PSA SCREENING?
- 5 WHY DO SOME RECOMMEND PSA SCREENING?
- 6 PROSTATE CANCER TISSUE BIOPSY
- 7 RISK CLASSIFICATION OF PROSTATE CANCER (D’AMICO RISK GROUPS)
- 8 TREATMENT OPTIONS (RELATIVE TO RISK GROUPS)
- 9 IMPORTANT SIDE EFFECTS OF TREATMENT TO KEEP IN MIND
- 10 ACKNOWLEDGMENTS
OVERVIEW
This page is dedicated to informing others about a few very important clinical pearls involving the topic of prostate cancer.
THE DIGITAL RECTAL EXAM (DRE)
How to perform a DRE is covered on the Genito-Urinary (GU) Exam page, however one critical point will be re-iterated here. When performing this exam it is important upon insertion to realize the anatomy of the anus/anal canal (depicted below).
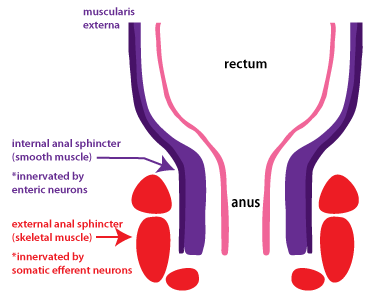
The external anal sphincter is composed of skeletal muscle that is innervated with pain receptors. It is for this reason that especially in the beginning of the DRE one must be very gentle and go slow. The inside of the anus contains only smooth muscle (that contains only pressure receptors and will not register pain).
*Regardless of the position the patient is in for the exam, make sure you have proper lighting for inspection and insertion. This (among other things) will enable you to avoid any hemorrhoids when performing the DRE.
CAUSES OF FALSELY ELVEATED PROSTATE SERUM ANTIGEN (PSA) LEVELS
While not known to all medical providers, there are various activities that MUST be avoided at least 1 week before a PSA screen (because they can falsely elevate the PSA):
- Ejaculation of any kind (intercourse, masturbation)
- Activities that apply pressure to the groin/prostate (bicycle riding, horseback riding)
- Activities that result in vibratory forces being transmitted to the body (operating heavy machinery, operating jackhammers)
- Medical interventions that can apply force to the prostate (such as insertion of a foley catheter)
- Medical processes that involve the prostate (such as benign prostatic hypertrophy, and prostatitis)

*Patients commonly are ignorant of the above causes of falsely elevated PSA. If you are referred a patient with a pervious PSA screen it is worth asking if they know about these cases of elevated PSA. Repeating the test may be worthwhile.
WHY DO SOME RECOMMEND AGAINST PSA SCREENING?
Not long ago the U.S. Preventive Services Task Force (USPSTF) recommend against the usage of PSA screening for the diagnosis of prostate cancer. While a controversial decision, let us analyze WHY this recommendation was made.
- Overdiagnosis: this refers to the diagnosis of prostate cancer in individuals who would never have been affected by their detected diseased.
- Overtreatment: this refers to the usage of overly aggressive therapy for patients who posses indolent forms of prostate cancer.
What can be done to address these concerns WITHOUT eliminating PSA screening all together? While the USPSTF brings up very valid concerns regarding the usage of PSA screening, there are alternative measures that can be taken to address these issues (without eliminating the usage of PSA screening).
- Addressing overdiagnosis: given that it has been shown that a prostate cancer diagnosis will not affect mortality until after 7 years post diagnosis, patients with a life expectancy lower then 7 years likely should not receive PSA screening (some physicians round this number up to 10 years).
- Addressing overtreatment: patients who are at low risk (depending upon stage and D’Amico risk group) can be enrolled in less aggressive treatment regimens (which can also include active surveillance)
WHY DO SOME RECOMMEND PSA SCREENING?
In light of the USPSTF recommendation against the usage of PSA screening, it is important to remember that both the American Urological Association (AUA) and American Cancer Society [glossary_exclude](ACS)[/glossary_exclude] recommend PSA screening because it has been shown to lower prostate cancer related deaths in patients. With this in mind the proper usage of PSA screening can help address the controversy that exists with regards to screening between organizations.
High risk groups for prostate cancer include (but are not limited to) African Americans, and those with a family history of the diseases (in first degree relatives). Generally speaking these individuals should receive a baseline PSA reading at age 35, and yearly PSA screens should be conducted starting at the age of 40.
Low/normal risk groups should establish a baseline PSA reading at the age of 40, and then yearly PSA screens should be conducted yearly starting at the age of 50.
*These are general guidelines and exceptions can always be made given the specific clinical context. It is important to keep in mind the complications that can arise form overdiagnosis and overtreatment of patients when considering PSA screening (discussed in the above section).
PROSTATE CANCER TISSUE BIOPSY
While prostate cancer is diagnosed and scored (i.e. Gleason score) based upon a tissue biopsy, it is important to realize its limitations. A few important factors to remember are that:
- Based upon the size of the prostate, as well as the size of the biopsy needle used, typically less than 1% of the total prostate tissue is biopsied.
- The anterior 2/3rds of the prostate are not accessible by the biopsy needle. Typically 15% of prostate cancers can be found in this anterior region of the prostate (and will never be biopsied given the length of the biopsy needle).
- Prostate cancer can be missed even with a biopsy!
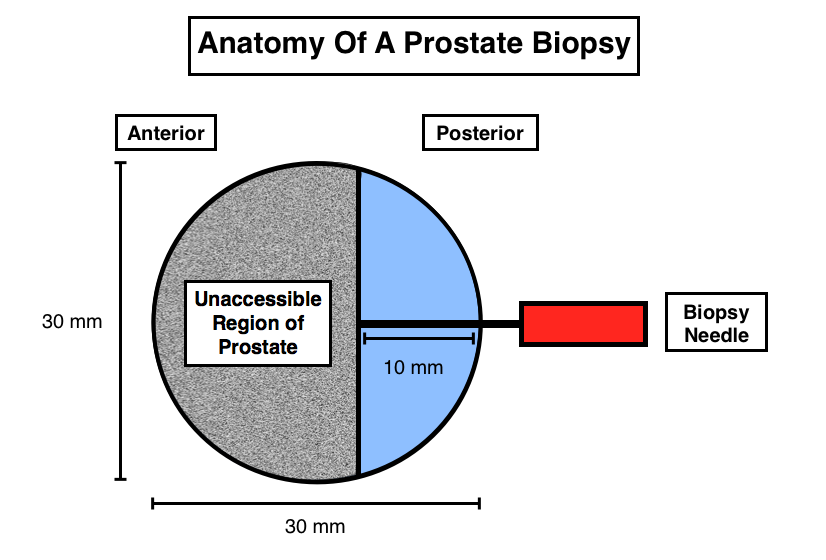
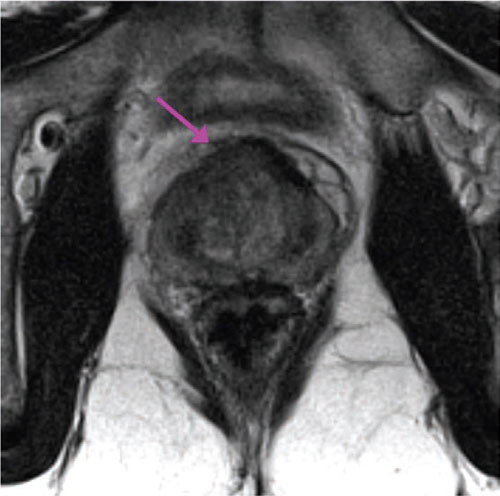
What if a PSA score is elevated by the Gleason score is low? For the reasons stated above, a discordance between a high PSA score that is associated with a low Gleason score tumor should warrant further investigation (even if a repeat biopsy confirms the initial Gleason scoring). Often times, higher grade prostate cancer can “hide” in the anterior portion of the prostate that is inaccessible to biopsy needles. In the patient scenario described above, a multiparametric MRI should be conducted to image the anterior portion of the prostate. This type of imaging looks at restrictive diffusion (how easily fluid can flow through a tissue) to help contextualize the nature of the tumor (the more dense/tightly packed with cells a tumor is, the less water will be able to flow thought the tissue/lower diffusion constant).
RISK CLASSIFICATION OF PROSTATE CANCER (D’AMICO RISK GROUPS)
A good initial step in characterizing prostate cancer (after a full examination that includes a DRE, PSA, biopsy, and any required imaging) is to risk stratify the patients. The D’Amico risk classification is a simple yet effective system that divides patients into three risk groups (low, intermediate, and high risk) regarding their likelihood of biochemical recurrence post treatment. It utilizes PSA, histology, and clinical stage.
Low Risk: all conditions must be met
- PSA ≤ 10
- Biopsy Gleason ≤ 6
- T1c or T2a clincial stage
Intermediate Risk: only one condition needs to be met
- PSA >10-20
- Biopsy Gleason 7
- T2b clinical stage
High Risk (bone scan and CT/MRI of pelvis should be acquired): only one condition needs to be met
- PSA > 20
- Biopsy Gleason 8-10
- T2c or higher clinical stage
*This is the initial step in characterizing the prostate cancer that a patient possesses. Followup evaluations (there are other prognostic factors) will help further contextualize the nature of the disease at hand.
TREATMENT OPTIONS (RELATIVE TO RISK GROUPS)
Generally speaking, there are only a few different treatment options that are available to patients who have prostate cancer: active surveillance, radical prostatectomy (RP), radiation therapy, and testosterone suppression (TS, a form of hormone therapy). Which treatment/combination of treatments one receives usually will depend on their risk category:
- Low Risk: these patients are able to enroll in active surveillance (especially if life expectancy is < 10 years) or seek active treatment (either RP/RT).
- Intermediate/High Risk: one treatment option for these patients is RT with TS or RP (with possible RT and TS to with follow up).
*It is important to realize that there is no randomized clinical trial comparing each treatment moodily against the rest. The decision with regards to which treatment option to pursue must be made with the side effects and the patient’s values in mind!
IMPORTANT SIDE EFFECTS OF TREATMENT TO KEEP IN MIND
While managing the prostate cancer is very important, it is only part of the battle. Managing the side effects of treatment options is also very vital to the overall well being of the patient (and these side effects NEED to be considered by the patient prior to the start of therapy).
Radical Prostatectomy holds the very likely risk of urinary incontinence and erectile dysfunction.
Radiation therapy carries the risk of erectile dysfunction, rectal bleeding, and a 1/300 chance of the development of a secondary cancer.
Testosterone suppression/hormone therapy can cause a wide variety of symptoms (severity and presentation can vary from patient to patient)
- Hot flashes
- Decreased Libido
- Metabolic Syndrome: increased cholesterol, blood pressure, glucose, and fat; decreased muscle, genitals, and body hair (except on scalp)
- Anemia
- Gynecomastia
- Increased cardiovascular events in men with pre-existing cardiovascular disease
*If on Hormonal Rx for > 1 year one might expect:
- Decreased Bone Mineral Density and increased fracture risk
- Depression
- Associations (not proven casual effects) with decreased mental acuity, decreased renal function, and increased Alzheimer’s disease
ACKNOWLEDGMENTS
A very special thanks goes to Dr. Anthony Victor D’Amico who made this page possible with his expertise.
Page Updated: 03.02.2016