Page Contents
- 1 WHAT IS IT?
- 2 WHAT CAUSES IT?
- 3 WHY IS IT A PROBLEM?
- 4 WHAT MAKES US SUSPECT IT?
- 5 CLINICAL WORKUP
- 6 WHEN ARE WE COMFORTABLE MAKING A DIAGNOSIS?
- 7 WHAT ELSE ARE WE WORRIED ABOUT?
- 8 HOW DO WE TREAT IT?
- 9 HOW WELL DO THE PATIENTS DO?
- 10 WAS THERE A WAY TO PREVENT IT?
- 11 OTHER HY FACTS?
- 12 ARCHIVE OF STANDARDIZED EXAM QUESTIONS
- 13 FURTHER READING
WHAT IS IT?
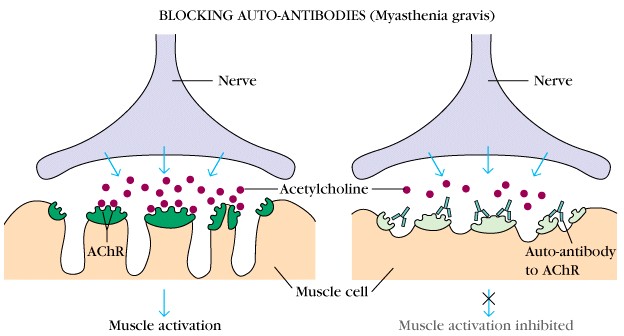
Myasthenia gravis is an autoimmune disorder (type II hypersensitivity reaction) that is characterized by damage of the acetylcholine receptor in the neuromuscular junction.
WHAT CAUSES IT?
Auto-antibodies that are formed against the acetylcholine receptor are ultimately to blame for this condition. Drug reactions (such as to the medication penicillamine) can cause this immune reaction in some patients, and often it is the thymus that is responsible for producing these auto-antibodies. Sometimes a thymoma is present, and is the underlying cause of this condition.
WHY IS IT A PROBLEM?
Destruction of these acetylcholine receptors will impair the ability to conduct acetylcholine mediated signaling to the muscles (impairing the body’s ability to contract its muscles). The end consequence of this will be muscle weakness (that worsens with usage). Muscles of the face are commonly involved, leading to double vision and a drooping eyelid(s).
WHAT MAKES US SUSPECT IT?
Risk factors:
Female sex
Initial presentation:
Chief Complaints:
- Drooping eyelid
- Double vision
- Limb weakness
History Of Present Illness:
Other presenting symptoms can include:
- Dysphagia
- Dysarthria
Symptoms are worsened with muscles use: often patient symptoms worsen throughout the course of the day as the muscle is used more and more.
Symptoms are sometimes reversed with slight rest: the course of patient symptoms is fluctuating. Resting for a few minutes may temporarily reverse the symptoms of the patient.
Physical exam:
HEENT exam:
- Ptosis that is often asymmetric
- Diplopia that often resolves when one eye is closed.
Motor exam can reveal weakness in the limbs that gets worse with fatigue. The most commonly affected muscles are:
- Dorsiflexors of the foot
- Deltoids
- Triceps
- Finger/wrist extensors
CLINICAL WORKUP
Ice pack test: NMJ transmission is more efficient at lower temperatures, if an ice pack is applied to the eyes improves ptosis can be observed. This may not be common clinical practice, but is an interesting fact that might be tested on standardized exams.

Tensilon test: Edrophonium (short acting indirect agonist of cholinesterase) administration historically was used to diagnose Myasthenia gravis if the patients symptoms improved with its administration. This medication will increase the levels of acetylcholine by inhibiting its breakdown, reversing muscles weakness in patients with myasthenia gravis.
Serology: this condition is ultimately diagnosed by the presence of anti-acetylcholine receptor antibodies or muscle-specific tyrosine kinase (MuSK) antibodies in the serum.
WHEN ARE WE COMFORTABLE MAKING A DIAGNOSIS?
Ultimately, the detection of antibodies against the acetylcholine receptor or MuSK will help confirm the diagnosis of myasthenia gravis.
WHAT ELSE ARE WE WORRIED ABOUT?
Myasthenic crisis: this condition is characterized by severe muscle weakness that leads to respiratory failure. It can be precipitated by various events (pregnancy, infection, surgery, medications) and is an emergency.
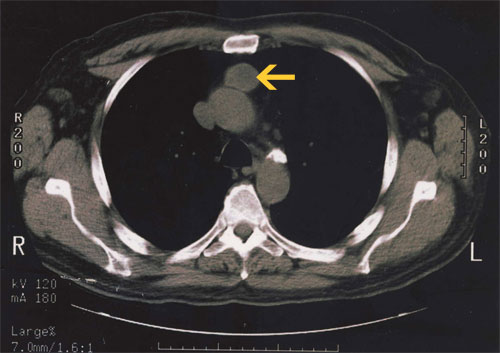
Thymoma is a benign tumor of the thymus tissue that is associated with Myasthenia gravis. The thymus is often the producer of the anti-ACh receptor antibodies. A CT scan/MRI should be done to investigate patients for a thymoma (and thymic hyperplasia can also be seen).
HOW DO WE TREAT IT?
Major goal of therapy is to help restore acetylcholine signaling: as a result anticholinesterases are used to increase the amount of acetylcholine in the NMJ. Options include:
- Neostigmine is an anticholinesterase which increases ACh levels and does not penetrate the CNS.
- Pyridostigmine is a long acting anticholinesterase which increases ACh levels and does not penetrate the CNS
- Corticosteroids
- Azathioprine
Thymectomy often is conducted to remove the source of the patient’s antibodies: this can be performed even in the absence of a clear thymoma.
HOW WELL DO THE PATIENTS DO?
The maximum severity of the disease is often reached within the first few years. This is a progressive disorder with no definitive treatment. A large fraction of patients progress to respiratory failure.
WAS THERE A WAY TO PREVENT IT?
N/A
OTHER HY FACTS?
Can present as a restrictive lung disease (because of poor muscular effort)
This is the most common neuromuscular junction disorder
ARCHIVE OF STANDARDIZED EXAM QUESTIONS
This archive compiles standardized exam questions that relate to this topic.
FURTHER READING
Page Updated: 08.01.2016