Page Contents
- 1 OVERVIEW
- 2 WHAT ARE LUNG OPACITIES?
- 3 GROUP 1: ALVEOLAR COMPARTMENT OPACITIES (AKA CONSOLIDATIONS)
- 4 GROUP 2: ATELECTASIS
- 5 GROUP 3: INTERSTITIAL COMPARTMENT OPACITIES (DISCRETE LINES)
- 6 GROUP 4: INTERSTITIAL COMPARTMENT OPACITIES (NODULES)
- 7 GROUP 5: AIRWAY COMPARTMENT OPACITIES
- 8 GROUP 6: DISCRETE LUNG NODULES (MASSES)
OVERVIEW
This section provides a clear algorithmic framework on how to approach thinking about lung opacities. This may seem like a very simple topic, however often times the basics regarding lung opacities on a chest X-ray are overlooked.
WHAT ARE LUNG OPACITIES?
It is important to first define what exactly a lung opacity is before discussing the algorithm we will use to think about them. In short, a lung opacity refers to an unexpected density over the area of the lungs on a chest X-ray (these will appear WHITE on the chest X-ray).
It is important to realize that there are a few major types of lung opacities that each have different features, and also different conditions that can be responsible for them.
- Alveolar compartment opacities: consolidations in the alveoli themselves make up a common cause of lung opacities.
- Atelectasis: collapse of the lung parenchyma can involve multiple compartments, and can often times present as a unique and distinct type of lung opacity.
- Interstitial compartment opacities (discrete lines): the interstitial space may be responsible for the opacities, however it is important to note the nature of opacities can be variable.
- Interstitial compartment opacities (nodules): the interstitial compartment may be filled with nodules that are responsible for the opacities on the chest X-ray.
- Airway compartment opacities: the airways themselves can be the source of the opacities on the study.
- Discrete nodules (single or multiple): the last category refers to lung nodules/masses that do not observe the normal boundaries of the lung compartments.
*While it is convenient to organize all opacities into these categories, it is important to remember that sometimes there can be more then one process going on at once (resulting in multiple types of opacities that can make interpretation slightly more challenging.
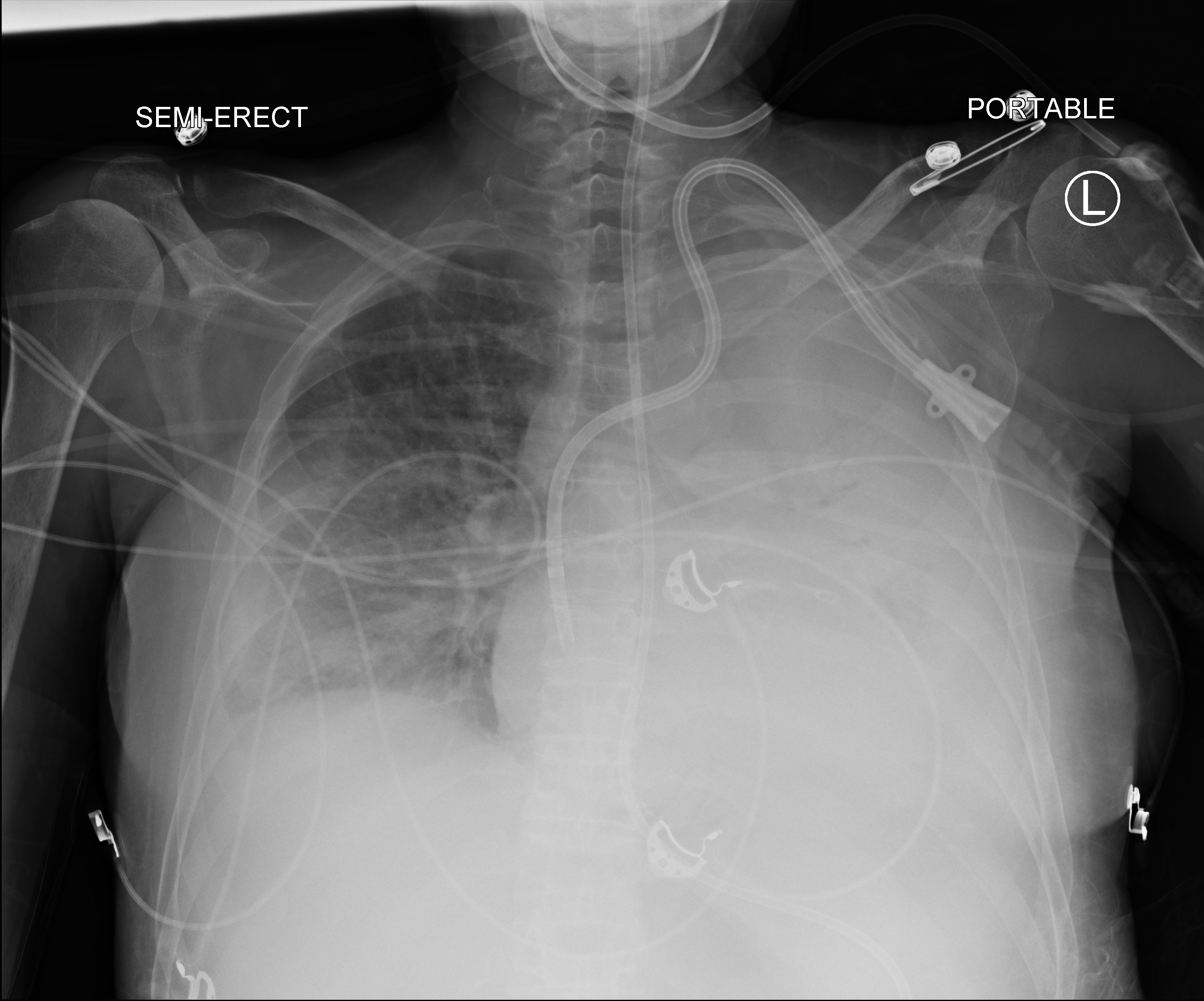
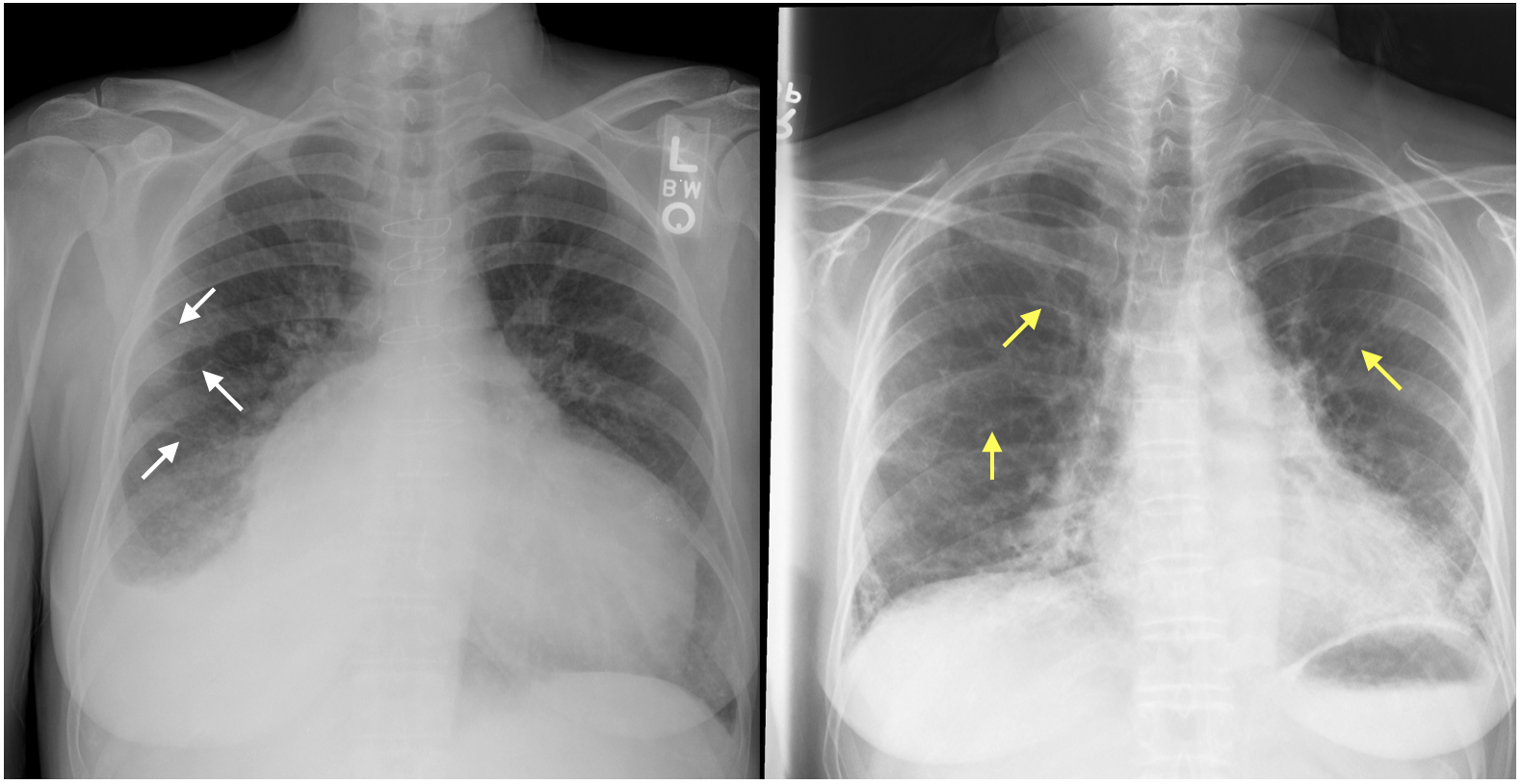
GROUP 1: ALVEOLAR COMPARTMENT OPACITIES (AKA CONSOLIDATIONS)
What are key features of this type of opacity?
- Air bronchograms: as airspaces of the lung will opacity they will create contrast with the air filled airspaces producing these air bronchograms.
- Confluent opacity: the opacity will be confluent in the affected area (between its borders).
- Fluffy/hazy periphery (not well defined edges): this will be the interphase between normal and abnormal regions of the lung tissue.
- Lack of volume loss: alveolar conditions do not present with volume loss like atelectasis.
Once you are thinking about alveolar opacities, it is important to contextualize its temporal nature (chronic vs. acute) as this will impact the differential.
What is the differential for this type of opacity (acute setting)?
- Focal distribution: pneumonia/aspiration, hemorrhage
- Diffuse: edema, acute lung injury, pneumonia, hemorrhage
What is the differential for this type of opacity (chronic setting)?
- Tumor: invasive mucinous adenocarcinoma, lymphoma
- Inflammatory: organizing pneumonia, chronic eosinophilic pneumonia, sarcoidosis
- Other: Lipoid pneumonia, alveolar proteinosis
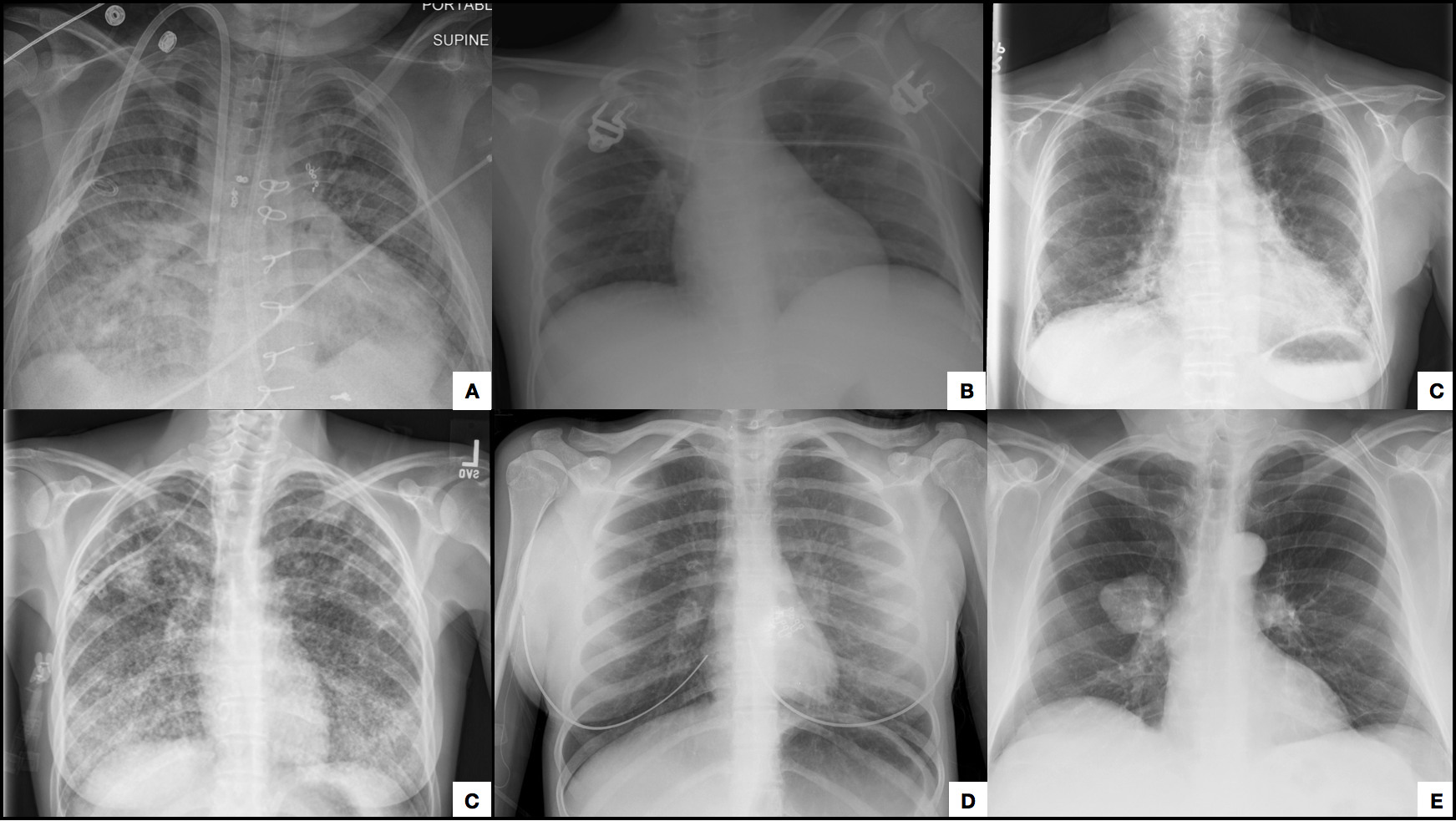
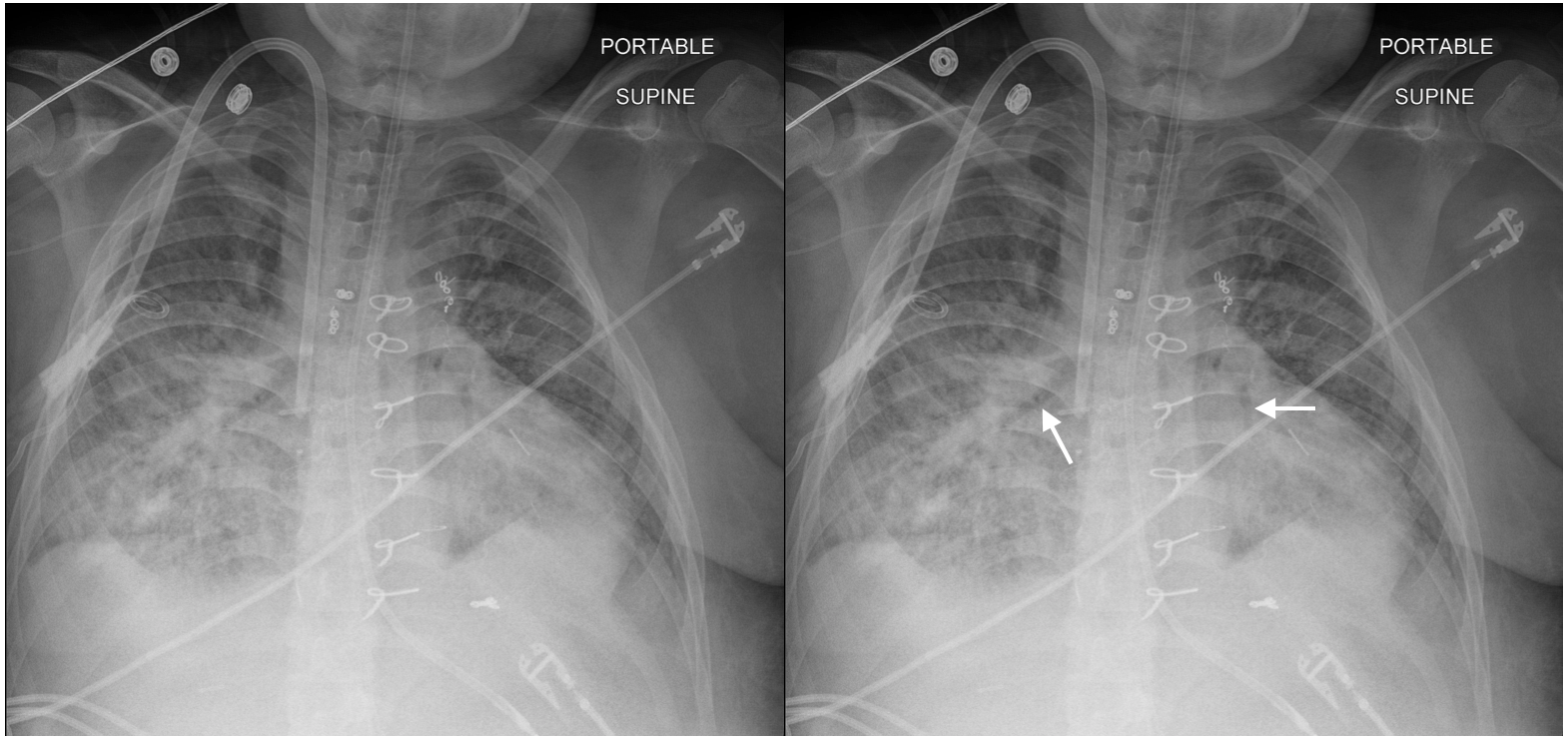
GROUP 2: ATELECTASIS
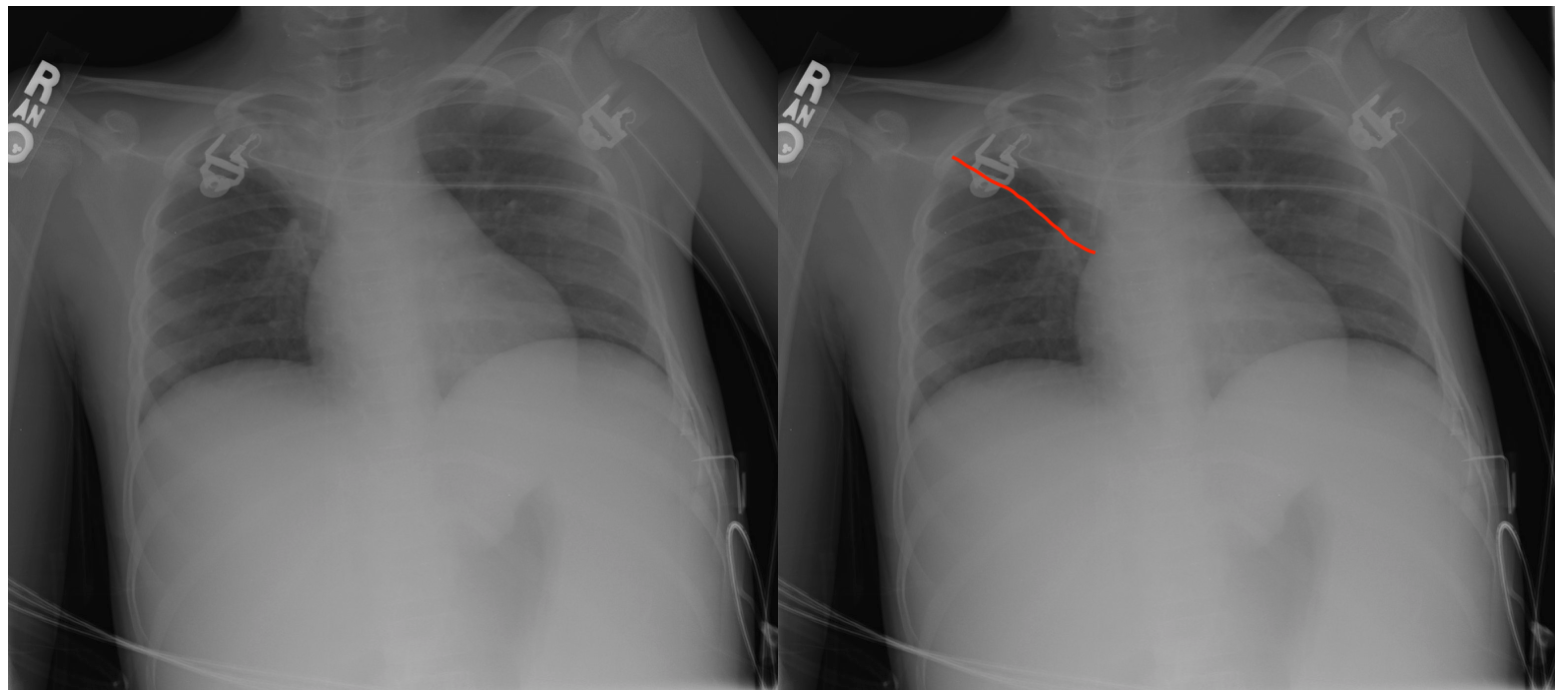
What are key features of this type of opacity?
- Confluent opacity: the opacity will be confluent in the affected area (between its borders).
- Signs of volume loss: this can include fissure displacement (most sensitive sign of volume loss), deviation of mediastinal structures, and an elevated diaphragm.
What is the differential for this type of opacity?
- Obstructive/resorptive: such as the obstruction of a bronchus
- Passive: compression of the lungs
- Cicatricial: related to scarring
- Adhesive: surfactant deficiency
GROUP 3: INTERSTITIAL COMPARTMENT OPACITIES (DISCRETE LINES)
What are key features of this type of opacity?
- Non-confluent opacities: the entire distribution of the opacity will not be confluent.
- Kerley B lines: for certain types of interstitial opacities
- Thick, wavy, and irregular lines: for conditions that result in fibrotic lungs.
What is the differential for this type of opacity (thin/Kerley B lines)?
- Thin lines (Kerley B lines): edema, malignancy
What is the differential for this type of opacity (thick, wavy irregular lines)?
- Lower lobe predominant: idiopathic pulmonary fibrosis, connective tissue disease, drugs, asbestosis, hypersensitivity pneumonitis
- Upper lobe predominant: Sarcoidosis, prior TB, prior fungal infection, pneumoconioses
GROUP 4: INTERSTITIAL COMPARTMENT OPACITIES (NODULES)

What are key features of this type of opacity?
- Very small nodules: can give the appearance of many little dots. Typically these are almost always interstitial.
- Non-confluent opacity: the entire distribution of the opacity will not be confluent given that their will be many dots separated in space.
- Diffuse distribution:
- Well defined nodules: typically interstitial nodules will be well defined. In some rare cases these can actually be alveolar nodules (if not well defined).
What is the differential for this type of opacity (hematogenous spread/random distribution on CT)?
- Miliary tuberculosis: can be one presentation of TB
- Miliary fungal infection: such as cocci
- Metastasis:
What is the differential for this type of opacity (lymphatic spread/perilymphatic distribution on CT)?
- Sarcoid:
- Metastasis:
- Penumoconioses: such as silica
GROUP 5: AIRWAY COMPARTMENT OPACITIES
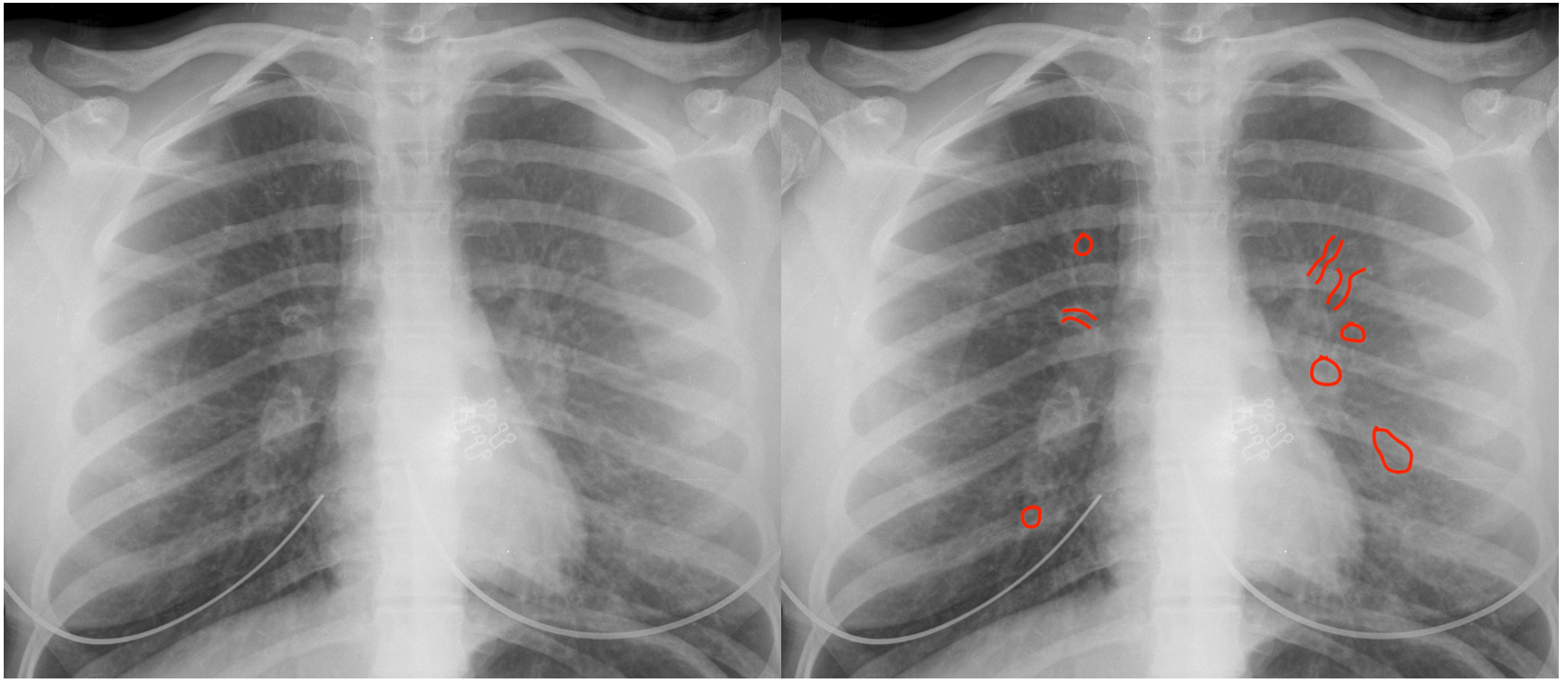
What are key features of this type of opacity?
- Circles/tubes with air/opacities: this can be a very characteristic pattern of airway disease. They can have thick or thin walls.
- Non-confluent: the entire distribution of the opacity will not be confluent.
What is the differential for this type of opacity (mild disease)?
- Asthma
- Viral infection
- Chronic bronchitis
What is the differential f:or this type of opacity (severe disease)?
- Bronchiolitis obliterans
- Immunodeficiency
- Ciliary dyskinesia
- Cystic fibrosis
- Allergic bronchopulmonary aspergillosis (ABPA)
- Tuberculosis
- Cartilage disease
GROUP 6: DISCRETE LUNG NODULES (MASSES)

What are key features of this type of opacity?
- Does not observe anatomic boundaries of compartments; these opacities will invade into surrounding structures.
What is the differential for this type of opacity?
- Granuloma
- Hamartoma
- Primary bronchogenic carcinoma:
- Metastasis
- Other: there are other casues however the majority will be those listed above.
What makes a nodule suspicious for malignancy?
- Large size: the larger, the less likely it is benign.
- Spiculated border: benign nodules will generally have a smooth border.
- No calcification/irregular calcification: benign nodules typically have diffuse calcifications.
- Growth over time: benign nodules should remain stable in size over time.
Page Updated: 07.27.2019