OVERVIEW
While tunneled hemodialysis catheters have much utility in medicine, and have some clear indications, there are some instances in which a tunneled hemodialysis catheter should not be placed. It is critical to remember that tunneled lines are NOT THE ONLY OPTION for patients who need dialysis and that non-tunneled temporary lines also are an option (and can be routinely placed on the floor outside of the IR suite). It is very useful to make sure that we always asks ourselves if patients being considered for a tunneled line may be better served by a non-tunneled dialysis catheter.
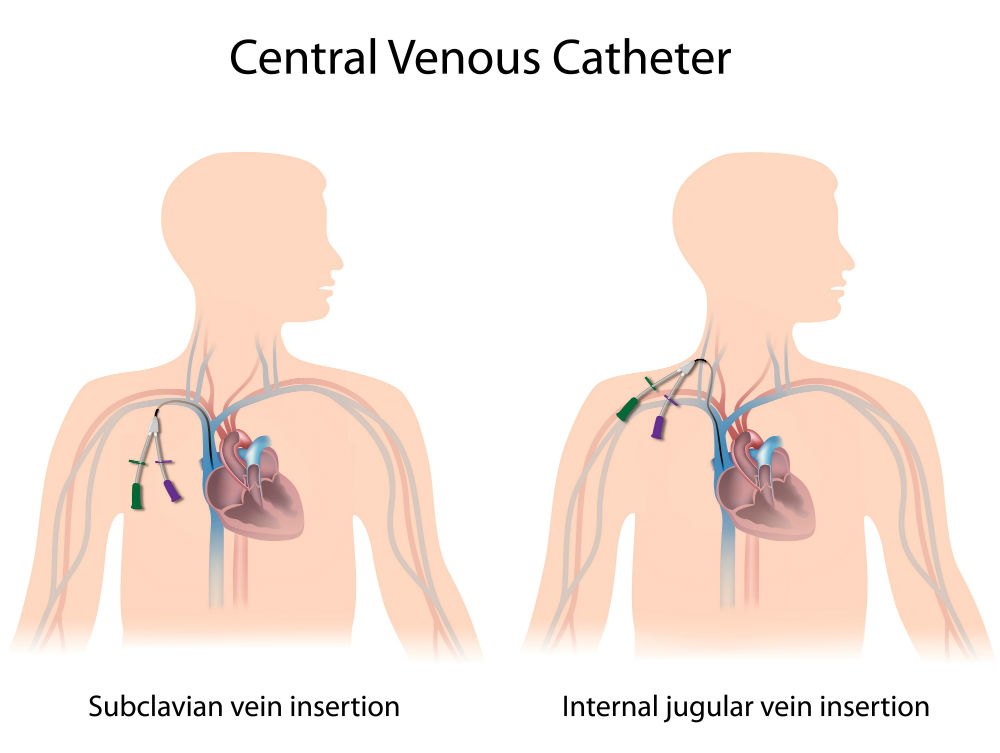
The main difference between these tunneled and non-tunneled lines really is the process of tunneling as well as some of the considerations that come with making trip to the IR suite (receiving moderate sedation for the procedure instead of just local anesthetic, extending a wire past the heart for the placement of the line fluoroscopically). These all add up to make the tunneled line a considerably more involved procedure compared to the placement of what is essentially just a traditional central line.
ABSOLUTE CONTRAINDICATIONS
There are a few instances where a tunneled catheter is very clearly not the right option for the patient (and that a non-tunneled line or other option for dialysis should be utilized). These are discussed in more detail below.

SEPSIS
In patients that have sepsis/bacteremia/a disseminated systemic infection a tunneled line is not appropriate. This is because the patient will have to have the line removed soon after they clear their infection. There is no reason to subject a patient to the process of tunneling a line just to have it removed shortly thereafter. In the cases of septic patients who need urgent dialysis a temporary line should be placed. Once the patient is no longer septic/infected this temporary line can be removed, the patient may have a line holiday in between dialysis treatments, and then can either have another temporary line placed or a tunneled line placed once they are no longer actively infected.
*It is not appropriate to place tunneled lines in actively infected patients
PATIENTS WITH INFECTIONS OVER THE SITE OF CATHETER ENTRY
An example of this can be a patient with cellulitis around where the catheter might be tunneled. The reasoning is similar to the sepsis example discussed above.
UNSTABLE PATIENTS
This can be a bit more subjective, however patients who are not stable enough to tolerate the tunneling procedure (given that it is more involved then simply placing a central line on the floor) should not be candidates for a tunneled catheter. Some providers will make the argument that most ICU patients should not be considered for tunneled lines given their relative instability. Here are some of the aspects that may make it not practical to place a tunneled line in an unstable patient:
- Inability to safety transport the patient: patients will need to be transported to the IR suite for the placement of the tunneled line (a regular non-tunneled line can be placed bedside). Patients with severe hemodynamic instability should remain in the unit under close monitoring.
- Patients unable to safely receive sedation: while not necessarily required for patients to receive a tunneled line (it is possible to do the tunneling procedure with just local lidocaine alone), generally if a patient is not stable enough to receive sedation safely then the argument can be made to place a temporary line and then place the tunneled line after the patient is more stable (also to spare them unnecessary discomfort).
- Inability to lie flat: some patients are not stable enough to lie flat for the amount of time that a tunneled line in the IR suite will require.
*In the end while a tunneled catheter has advantages over a non-tunneled line, the safety of the patient can not be comprised. Non-tunneled lines can always be placed initially and then converted to tunneled lines when the patient is more medically optimized.
RELATIVE CONTRAINDICATIONS
Some contraindications are not as absolute as the ones discussed above and may instead be slightly more subjective. Here are some of those contraindications that should be taken into consideration when considering placing a tunneled line in a patient.
COAGULOPATHY
Patients are at higher risk for bleeding from a tunneled line, simply because of the actual tunneling process that involves tunneling the line through the subcutaneous tissues. Generally speaking patients who have an INR > 1.5 and a platelet count < 50,000 µL should have these values corrected prior to the procedure.
This can become more challenging for patients who have a coagulopathy that is not correctable with blood products and who may still require longer term dialysis access. These values are not always strict cutoffs and exceptions may be made.
ELECTROLYTE ABNROMALITIES
Patients who require dialysis urgently may also have severe electrolyte abnormalities (such as hyperkalemia). These patients may benefit from having a temporary line placed first so that their electrolyte status may be optimized before the more involved tunneled line is placed.
Given that electrolyte abnormalities increase patient risks for arrhythmias (with can be precipitated by passing a guide wire past the patient’s heart during an IR guided line placement) it is important to make sure we minimize the procedure risk we expose patients to.
Page Updated: 03.31.2019