Page Contents
OVERVIEW
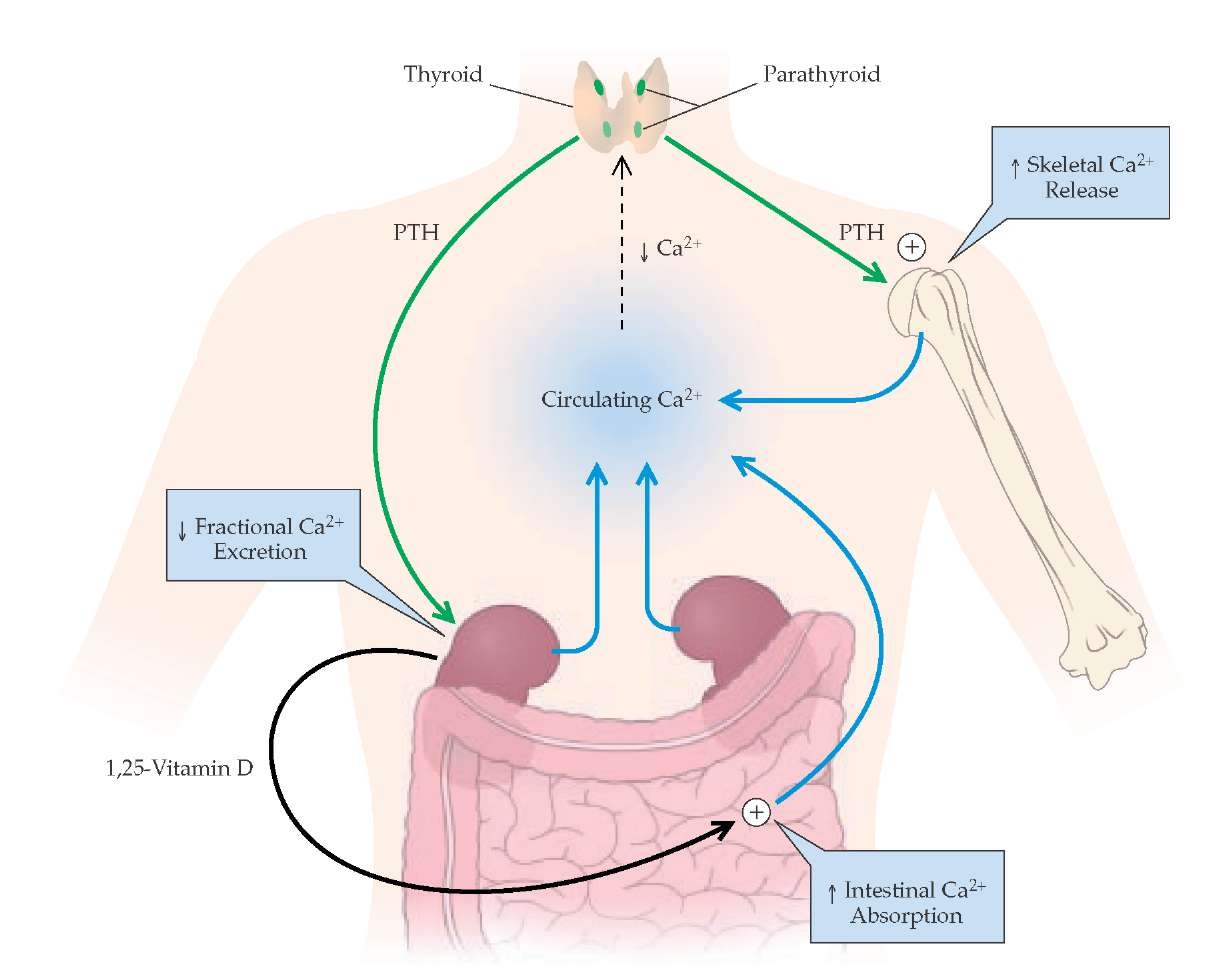
This page focuses on the hormonal pathways that control the production of parathyroid hormone (PTH). PTH is a small peptide hormone that is produced and secreted by the parathyroid gland. It is fast acting to maintain levels of ionized calcium in the blood.
WHAT INDUCES PTH SECRETION?
Decreased calcium concentration: This is mediated by a calcium sensing receptor (CaR) on the surface of the parathyroid. This relationship is sigmoidal at physiological levels of calcium so that it can be maintained easily (small changes in calcium => large changes in PTH).
MODERATE hypomagnesemia: magnesium is needed for PTH secretion, and moderate levels of hypomagnesemia will stimulate PTH secretion.
Hyperphosphatemia: high levels of phosphate in the blood will increase the complexed fraction of calcium causing hypocalcemia => PTH secretion.
WHAT REPRESSES PTH SECRETION?
Increased calcium concentration: This relationship is sigmoidal at physiological levels of calcium so that it can be maintained easily (small changes in calcium => large changes in PTH).
SEVERE hypomagnesemia: magnesium is required for PTH secretion, and severe depletion of magnesium will inhibit the ability of the parathyroid to secrete PTH.
Hypermagnesemia: paradoxically, too much magnesium will also inhibit PTH secretion by the parathyroid. This is because magnesium itself can bind to the CaRs (inactivating them at high concentrations).
Hypophosphatemia: low levels of phosphate in the blood will decrease the complexed fraction of calcium causing hypercalcemia => inhibited PTH secretion
Vitamin D: High levels of vitamin D (1, 25(OH)2D/calcitriol) will repress the expression of the PTH gene.
WHAT DOES PTH ACTUALLY DO?
PTH works to modulate calcium movement between the intestines, bones, and kidney.
- Bone: In the presence of permissive amounts of vitamin D (calcitriol), PTH stimulates bone resorption and release of calcium and phosphate into the ECF via an increase in the number and activity of osteoclasts (indirectly via an increase in osteoblast RANK ligand).
- Intestines: The effect of PTH on intestinal calcium absorption is indirect, via increased renal production of calcitriol, the active vitamin D metabolite, which promotes calcium (and phosphate) absorption.
- Kidney: PTH serves to increase the amount of calcium resorbed though the kidneys, while increasing the amount of phosphate excreted in the urine. PTH also acts to aid in the synthesis of calcitriol in the kidneys.
Page Updated: 02.21.2016