Page Contents
OVERVIEW
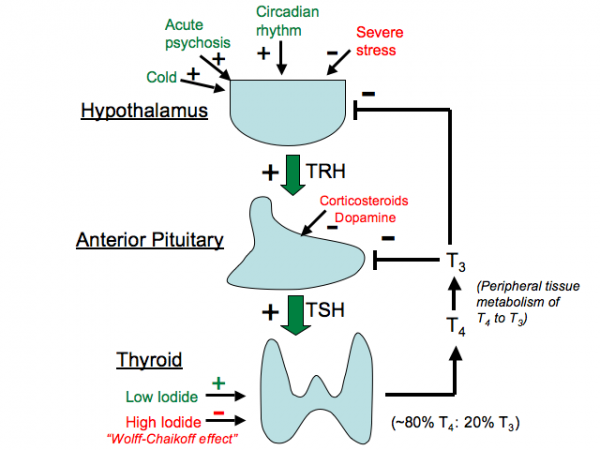
This page focuses on the hormonal pathways that control the production of thyroxine (T4) and triiodothyronine (T3). These thyroid hormones are important for setting the bodies base metabolic rate, and are responsible for many different physiological processes systemically.
Aside from serving an important player in fetal development, the thyroid has important roles in heart function, metabolism, and growth (among others that will be discussed later). As a result the signaling pathway below is very clinically relevant:
TRH (hypothalamus) => TSH (pituitary) => T4 (thyroid) => T3 (peripheral conversion) => target physiology
HYPOTHALAMUS
The hypothalamus starts off this hormonal pathway by the release of thyrotropin releasing hormone (TRH) which in turn acts upon the anterior pituitary to further propagate this signaling pathway.
Factors that increase TRH secretion include the following:
- Cold temperatures
- Pregnancy
- Circadian Rhythms
Factors that decrease TRH secretion include the following:
- T3/T4 hormones (negative feedback)
- Stress
ANTERIOR PITUITARY
The anterior pituitary continues this signaling pathway by releasing thyroid stimulation hormone (TSH)/thyrotropin. TSH works on the the thyroid to increase production of thyroid hormones (T4/T3). The mechanism by which TSH stimulates hormone production is by regulating Sodium/Iodine symporters in the thyroid. More TSH => more transport of iodine into the thyroid => more hormones production. *TSH is required for hormone production.
Factors that increase TSH secretion include the following:
- TRH
Factors that decrease TSH secretion include the following:
- T3/T4 hormones (negative feedback)
- Loss of TRH
THYROID
The thyroid gland is the organ that is responsible for producing the literal thyroid hormones (T4/T3). It mainly produces T4 which then is released into the blood stream.
Factors that increase T4 secretion include the following:
- TSH
- Appropriate levels of iodine
Factors that decrease T4 secretion include the following:
- T3/T4 hormones (negative feedback)
- Lack of iodine (this is required for production of T4)
- Very high dose of iodine (Wolff-Chaikoff effect, excess iodine temporarily inhibits thyroid peroxidase)
THYROID HORMONES IN THE BLOOD
What happens to T4 when it is released by the thyroid? While both T3 and T4 are in fact produced by the thyroid, for our purposes let us focus on the fact that the thyroid mainly produces and secretes T4. Here is a quick flow of what happens.
1.) T4 circulates in the blood bound to protein: the T4 hormone will circulate in the blood by binding to thyroxine binding globulin (TBG). As is the case with other hormones, there are bound (biologically inactive) and unbound (biologically active) fractions of T4 in the blood. Clinically we can measure the unbound fraction which is more physiologically relevant
- T3 can also bind TBG but not as strongly.
- T4/T3 are more stable when bound to TBG.
- Other proteins (ex albumin) also bind T4/T3 (but not as much).
- TBG is synthesized in the liver (hepatotoxicity decreases TBG synthesis), and estrogen can elevate its levels. Pregnancy and birth control can increase TBG => total T4 levels which is why only “free” T4 is measured clinically.
2.) At target tissues T3 is made: Once T4 reaches its target tissue destination, the expression of the proper deiodinases can convert it into T3 (the form of the hormone that actually serves a direct mechanistic role).
- This allows for tight control of T3 levels in the peripheral tissues.
- Type 1 and 2 deiodinases turn T4 into T3
- Type 3 deiodinases inactivate T3 by converting it into T2.
- Certain diseases can disrupt the balance of Type 1/2 vs. 3 deiodinases which will change effective levels of T3.
3.) T3 is transported into the cells: T3 does not enter the cell passively but is actively transported. One T3 transporter, the monocarboxylate transporter 8 (MCT8), has been identified to date. When mutated it causes severe neurologic disease in affected children (Allen-Herndon-Dudley Syndrome).
ACTIVITY OF T3 WITHIN THE CELL
Upon being transported into the target cell, T3 serves an important function. T3 binds thyroid hormone receptors (TRs) which are a type of nuclear hormone receptor. The TRs are transcription factors that mediate their effects by binding to the regulatory regions of target genes and turning them on or off. TRs have a specific DNA-binding domain that is similar to other nuclear receptors and a unique ligand-binding domain.
- In the absence of T3, the TRs are bound by proteins termed corepressors which repress gene transcription by changing histone and chromatin structure. This means that in the absence of T3, TRs still bind DNA but act to silence genes.
- T3 causes the TR to release corepressors and to then recruit coactivator proteins that activate gene expression. Thus, T3 controls what proteins the TR recruits in a particular cell.
- There are multiple isoforms of TR that can vary based upon a tissue specific manner (which can lead to tissue specific responses of T3).
FUNCTION OF T3 SYSTEMICALLY
The expression of TRs will in part dictate how T3-TR mediated signaling brings about physiological changes. With that in mind, this signaling pathway is important for a variety of different things.
1.) Development: Thyroid hormones are absolutely required for normal human development both in utero and as infants. Without normal thyroid hormone production early in life severe neurologic dysfunction can develop. This is why neonatal screening programs for hypothyroidism exist throughout the world.
2.) Growth: Intact thyroid signaling is important for normal skeletal growth in children. T3 has specific actions on the pituitary to increase growth hormone secretion and also acts on bone directly and influences growth and bone formation. In adults long-standing hyperthyroidism can lead to bone loss or osteoporosis.
3.)Metabolism: Thyroid Hormone signaling increases energy expenditure by a variety of mechanisms.
- Increases mitochondrial function (increasing uncoupling protein expression).
- Regulates (likely increases) Na+ K+ ATPase expression which regulates ATP breakdown and energy expenditure.
- Increases oxygen consumption and carbon dioxide production systemically.
4.) Cardiovascular System: T3 impacts cardiac function by regulating ion channel and myosin heavy chain gene expression. T3 also may regulate β-adrenergic receptor number and sensitivity to adrenergic signaling. Increased T3 will increase the heart rate and contractility (and vice versa).
5.) CNS Function: T3 is absolutely required for normal CNS development in utero and during childhood development. T3 is also required for normal hearing and color vision in mice. In adults T3 influences global CNS function and is a strong stimulator of the sympathetic nervous system.
6.) Cholesterol and Triglyceride Metabolism: T3 is a potent regulator of cholesterol metabolism and is an effective LDL-cholesterol lowering agent (enhances both the clearance of cholesterol from the blood, and its conversion to bile). T3 stimulates lipogenesis (which increases fatty acid and tri-glyceride synthesis).
7.) Glucose metabolism: T3 regulates hepatic glucose output but also regulates insulin metabolism, thus its effects on glucose metabolism are not straightforward. T3 regulates gluconeogenic gene expression and thus low levels could rarely be associated with low blood glucose levels. However, this is not common clinically.
Page Updated: 02.20.2016