Page Contents
- 1 VIDEO INTRODUCTION
- 2 WHAT IS IT?
- 3 WHY IS IT A PROBLEM?
- 4 WHAT MAKES US SUSPECT IT?
- 5 HOW DO WE CONFIRM A DIAGNOSIS?
- 6 HOW DO WE RULE OTHER DIAGNOSES OUT?
- 7 HOW DO WE TREAT IT?
- 8 HOW WELL DO THE PATIENTS DO?
- 9 WAS THERE A WAY TO PREVENT IT?
- 10 WHAT ELSE ARE WE WORRIED ABOUT?
- 11 OTHER HY FACTS?
- 12 ARCHIVE OF STANDARDIZED EXAM QUESTIONS
- 13 FURTHER READING
VIDEO INTRODUCTION
WHAT IS IT?
Diabets insipidus (DI) refers to a hormonal condition where there is an inadequacy of anti-diuretic hormone (ADH)/vasopressin signaling within the body. This can happen in one of two (general) ways.
- Central DI: this refers to a production/release issue of ADH from the pituitary/hypothalamus (decreased ADH)
- Nephrogenic DI: while ADH is properly made, the kidneys themselves do not respond to the ADH (increased ADH)
Some Causes: lithium and demeclocycline toxicity (nephrogenic), head trauma (central)
WHY IS IT A PROBLEM?
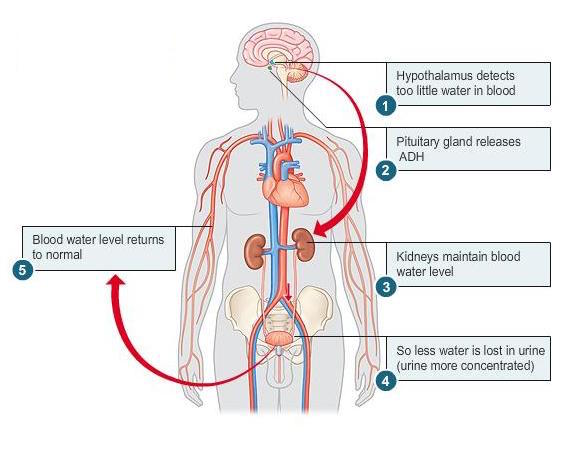
ADH is a very important hormone for regulating water resorption in the kidneys. As this signaling pathway is lost (either because of a lack of production, or because the kidneys are unresponsive to it) an individual is not able to re-sorb as much water in collecting ducts of the kidney leading to frequent urination of high volumes, and hypovolemia.
WHAT MAKES US SUSPECT IT?
Risk factors: family history (X-linked cause of diabetes insipidus exists)
Chief complaint: intense thirst (polydipsia and polyuria)
HOW DO WE CONFIRM A DIAGNOSIS?
Findings in all types of DI:
Urine values: low urine osmolality and specific gravity will be seen in DI simply because the body can not concentrate the urine.
Blood values: hypernatremia and high serum osmolality possible (due to diminished water resorption)
Water deprivation test: decreasing water intake will NOT result in increased urine concentrations.
How to distinguish between central and nephrogenic DI:
ADH levels: ADH will be decreased in central DI (production issue) and increased in nephrogenic DI
Response to ADH: only patients with central DI will respond to the administration of ADH clinically (either with general urine concentration, or during a water deprivation test). Typically one would expect about a 50% increase in the urine osmolarity.
HOW DO WE RULE OTHER DIAGNOSES OUT?
If the patient still cannot concentrate urine during periods of fluid restriction, this finding will rule out many other diseases (such as primary polydispia).
Furthermore, other conditions that might also present like DI (such as diabetes mellitus) can be ruled out given initial findings of low urine osmolality (because diabetes mellitus will present with large amounts of glucose in the urine.
HOW DO WE TREAT IT?
Nephrogenic DI
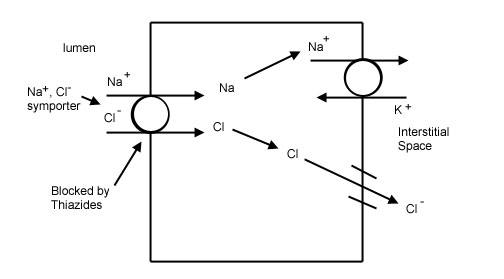
Thiazide diuretics (hydrochlorothiazide/HCTZ): while counterintuitive that one would give a diuretic for such a condition, this is to balance the loss of water with also the loss of solutes/salts. Losing only water due to deficiency of ADH signaling will not turn on the renin–angiotensin–aldosterone system (RAAS), however the loss of both water and salt (thanks to the added diuretic) WILL cause activation of the RAAS system. Activating RAAS will increase salt/water resorption in other areas of the nephron, helping in part restore the volume status of the patient.
Amiloride: Amiloride works by directly blocking the epithelial sodium channel (ENaC) which ends up inhibiting sodium reabsorption in the distal convoluted tubules, connecting tubules, and collecting ducts in the kidneys. It is a potassium sparing diuretic (potassium is not secreated in the urine) and it blocks the resorption of lithium (which is why it is often used for patients who are taking lithium for bipolar disorder).
Indomethacin: this is a is a nonselective inhibitor of cyclooxygenase (COX) 1 and 2, enzymes that usually contribute in prostaglandin synthesis from arachidonic acid (it is a NSAID). While the mechanism is not completely understood, blocking this pathway helps with symptoms of nephrogenic DI and reduces diuresis/levels of sodium in the serum.
*Hydration!
Central DI
Desmopressin (this is synthetic ADH) can be given to patients with central DI. Replacing the missing hormone makes sense!
*Hydration!
HOW WELL DO THE PATIENTS DO?
This depends entirely on the cause of the condition. Some causes are more serious than others.
WAS THERE A WAY TO PREVENT IT?
Drug induced causes of nephrogenic DI can be avoided by using medications without kidney toxicity (however this may not always be clinically possible).
WHAT ELSE ARE WE WORRIED ABOUT?
Hand–Schüller–Christian disease: this is a malignancy of Langerhans cells (antigen presenting immune cells of the skin/mucosa) that can infiltrate the pitutiary stalk and cause central DI.
Bipolar disorder: patients who are taking lithium for bipolar disorder can present with nephrogenic DI. Make sure to keep in mind the aspect of managing medications for bipolar disorder as well if such a patient presents with DI.
OTHER HY FACTS?
Damage to the posterior pituitary only produces TRANSIENT central DI (because the hypothalamus can still make ADH, and eventually it can also release it). If someone presents with chronic central DI, very likely the issue lies with the hypothalamus.
More causes of central DI: Pituitary tumor, autoimmune destruction, trauma, surgery, ischemic encephalopathy, idiopathic
More causes of nephrogenic DI: Congenital (ADH receptor mutation), as a result of hypercalcemia, lithium toxicity, demeclocycline (ADH antagonist) usage
*There are a variety of medications that can cause DI (read more here)
ARCHIVE OF STANDARDIZED EXAM QUESTIONS
This archive compiles standardized exam questions that relate to this topic.
FURTHER READING
Page Updated: 01.26.2016