Page Contents
OVERVIEW
This page is dedicated to organizing various examples of standardized exam questions whose answer is Guillain-Barré syndrome (GBS). While this may seem a odd practice, it is useful to see multiple examples of how GBS will be characterized on standardized exams (namely the boards and the shelf exams). This page is not meant to be used as a traditional question bank (as all of the answers will be the same), however seeing the classic “test” characterization for a disease is quite valuable.
KEY CHARACTERISTICS OF THIS CONDITION (ON EXAMS)
When it comes to standardized exams, each condition has its own “code” marked by key buzzwords, lab findings, clues, etc. If you are well versed in this code you will be able to more quickly identify the condition that is being discussed, and get the right answer on the exam you are taking. Below is the “code” for GBS.
Chief Complaints:
- Ascending pattern of muscle weakness that often affects the legs first and then climbs up the body. This occurs and progresses rapidly (days/weeks)
- Ascending pattern of tingling sensation/numbness can be associated with the muscle weakness (also will be rapid in nature)
- Difficulty walking can be the resulting complaint from the weakness
Patient History:
- Recent infection: sometimes the patient will have an upper respiratory illness recently (a few weeks before presenting) or a GI illness (diarrhea).
Clinical Workup:
- Decreased muscle strength will be noted on the physical exam
- Impaired sensation (all types) might be noted on the physical exam
- Absent/decreased deep tendon reflexes is almost always present
- Yellow (Xanthochromic) CSF can be seen on a spinal tap. Elevated protein is also a common finding in the CSF
- Slow conduction velocity will be noticed on nerve conduction studies
QUESTION EXAMPLES
Question # 1
A 40-year-old woman is brought to the clinic because of a tingling sensation in her fingers and toes for 3 days, and a rapidly progressive weakness in both of her legs. Her past medical history is notable for an upper respiratory tract infection 2 weeks ago. She explains that due to her weakness she was unable to get up from bed this morning without help from her boyfriend. A physical examination demonstrates weakness of all four extremities, distal greater than proximal. Her deep tendon reflexes are absent. Sensation is mildly decreased over the feet. What is the likely diagnosis?
Explanation # 1
Recent respiratory infection + rapid ascending weakness + loss of deep tendon reflexes = GBS
Question # 2
An otherwise healthy 28 year old male is brought to the ER because he has been experiencing a 3 day history of progressive weakness and pain in his lower extremities. Recently today he has noticed difficulty rising from a chair and climbing stairs. His vitals are within normal limits. A neurological exam shows significant weakness in the lower extremities (both proximally and distally) and there is weakness of the intrinsic hand muscles on both sids. His deep tendon reflexes are absent thought the body. What is the likely diagnosis?
Explanation # 2
Rapid ascending weakness + loss of deep tendon reflexes = GBS
Question # 3
A 35 year old male is brought to the clinic because he has been experiencing weakness and tingling that began in his feet, and now has reached his thighs. His symptoms began about 10 days ago and seems to worsen every day. A physical exam reveals decreased strength in his legs bilaterally. Patellar deep tendon reflexes are absent bilaterally as well. His past medical history is unremarkable with the exception of a respiratory infection that he had 16 days day. What is the likely diagnose sin this patient?
Explanation # 3
Rapid ascending weakness + loss of deep tendon reflexes + recent respiratory infection = GBS
Question # 4
A 30 year old male presents to the emergency room with difficulty walking for the past 3 days. He explains that he also feels an odd “tingling” in his feet as well. A physical eval reveals decreased strength in the lower extremities bilaterally. He also has absent deep tendon reflexes in both of his legs. His past medical history is unremarkable except for an episode of diarrhea that he experienced a couple of weeks ago that resolved on its own. What is the likely diagnosis in this patient?
Explanation # 4
Decreases strength in lower extremities + loss of deep tendon reflexes + recent GI infection (diarrhea) = GBS
Question # 5
A 25 year old male comes to clinic because he has been noticing a progressive numbness in both of his feet that has now risen to the level of his knees. Over the past day he has also noticed numbness and tingling in his hands. A physical exam reveals an ataxic gains, and his deep tendon reflexes are decreased in the upper extremities, and absent in the lower extremities bilaterally. Sensation to vibration is absent in his fingertips and feet bilaterally. He has moderate weakness in his distal upper extremities, and distal lower extremities. What is the likely diagnosis in this patient?
Explanation # 5
Rapid ascending numbness + loss of deep tendon reflexes + decreased sensation + decreased strength = GBS
Question # 6
A 35 year old woman comes both clinic because she has noticed a progressive weakness and numbness in all of her extremities. These symptoms began 4 days ago and have been getting worse each day. A physical exam reveals distal and proximal weakness in all of her extremities. Sensation to join position is decreased in her toes and fingers. Her deep tendon reflexes are absent in all extremities. Nerve conduction studies are performed and show slow conduction velocity in various nerves in her extremities. What is the likely diagnosis in this patient?
Explanation # 6
Rapid ascending weakness and numbness + loss of deep tendon reflexes + decreased sensation + decreased strength + slow conduction velocity of nerves = GBS
Question # 7
A 15 year old female is brought to the ER because she has a 3 day history of increasing weakness in her legs. She has also noticed numbness in her legs as well. Her past medical history is unremarkable except for a mild illness last week that was thought to be the flu. Her temperature is currently 98.8°F, pulse is 80 bpm, respiration’s are 22/min and her blood pressure is 120/80 mm Hg. A physical exam reveals a muscle strength of 2/5 in the lower extremities bilaterally. She has has decreased pinprick sensation along her lower extremities. Deep tendon reflexes in her legs are decreased. A lumbar puncture is performed and reveals a total protein concentration of 85 mg/dL and a white count of 3/mm³. What is the likely diagnosis in the patient?
Explanation # 7
Rapidly progressing weakness + decreased deep tendon reflexes + decreased sensation + recent flu-like illness + elevated protein in CSF = GBS
Question # 8
A 40 year old male comes to the clinic because he has noticed progressive weakness over the past few days. His weakness began at his feet and now has spread to the proximal aspects of his lower extremities. Over the past 24 hours he has also noticed weakness in his hands and face. His past medical history is non-contributory except for a recent upper respiratory illness that wa diagnosed about 2 weeks ago. A physical exam shows moderate weakness in his facial muscles, and more significant weakness in his extremities. His is areflexic. Sensation to light touch and vibration is decreased over his hands and feet. What is the likely diagnosis in this patient?
Explanation # 8
Rapidly progressing weakness + absent deep tendon reflexes + decreased sensation + recent respiratory illness = GBS
TESTABLE FACTS ABOUT THIS CONDITION (BEYOND ITS IDENTIFICATION)
Many questions on standardized exams go beyond simply recognizing the underlying condition. Often there are specific testable facts regarding some aspect of the disease’s pathophysiology/management/clinical implications that are commonly asked. Some of these are listed below:
Cause:
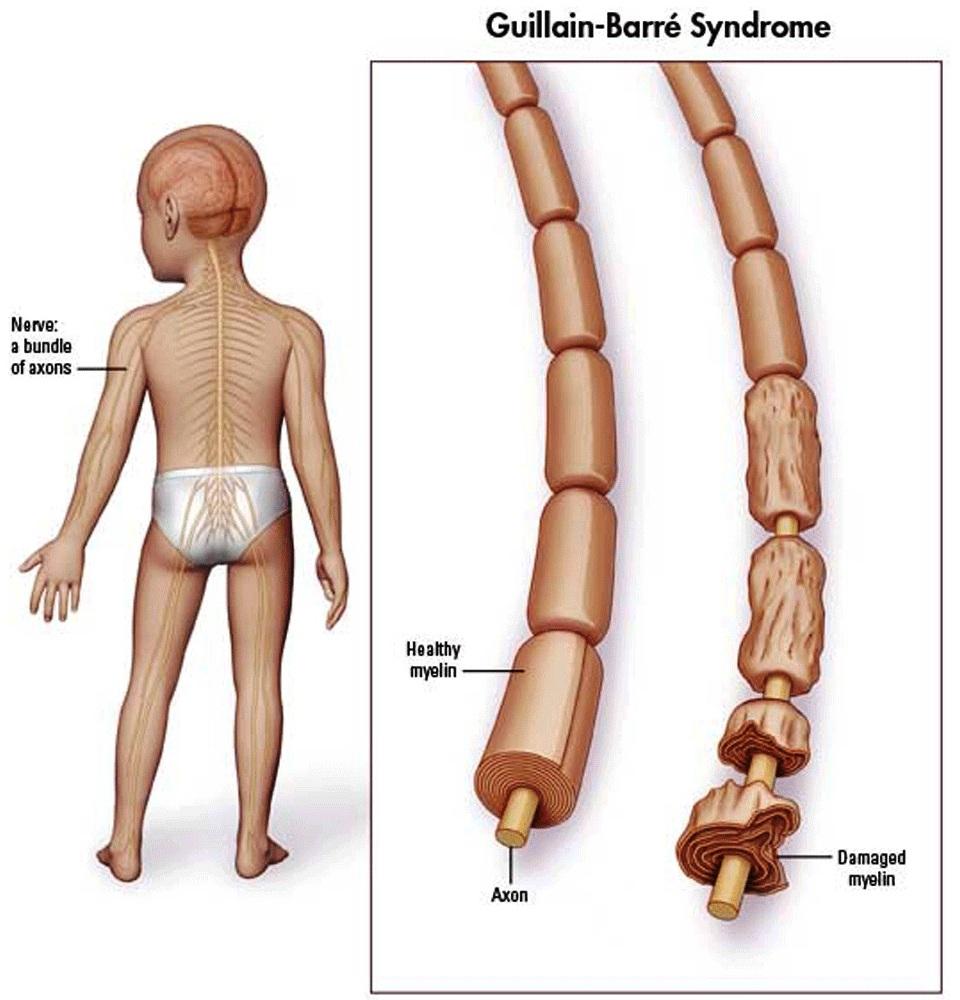
- Autoimmunne condition: results in the demyelination of the peripheral nerves.
- Precipitated by infection: usually either respiratory or GI infection. Infection with Campylobacter jejuni is the most common culprit (very testable fact)
- Impairs sodium gated sodium channels associated with statutory conduction along the length of the nerve
- Results in decreased nerve conduction velocity
Treatment:
- IVIG is used to neutralize autoantibodies.
- Plasma exchange might be necessary for more serious cases.
Page Updated: 01.18.2018