Page Contents
OVERVIEW
Conduct in numerical order (the order in which you would present the patient).
CN I (OLFACTION)
Initially inquire if their have been any issues/changes with the ability to taste and/or smell. If yes conduct the test.
– Have patient close eyes and one nostril.
– Use soap in room to test each nostril independently (can patient smell soap and identify what it is?)
– Repeat with the other nostril
CN II (VISION AND VISUAL FIELDS)
First test the visual acuity of the patient with correction (each eye should be tested independently).
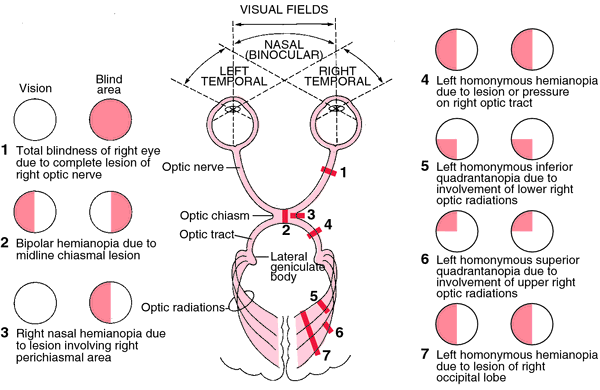
Visual fields: next the visual field of each eye (independently) should be tested. It is most important to test all 4 quadrants of each eye (either by using 1,2, 5 fingers or wiggling fingers).
– When patient initially closes eyes, one can ask the patient to look at them and ask them “Can you see my whole face? Are any parts blurry or missing?”
-Test 4 quadrants as described above. Vision is not lost on the periphery neurologically, rather in specific quadrants.
Without the patient moving their eye (keeping focus on your nose) move your hand (keeping it equidistant between you and the patient) into each quadrant and assess the integrity of the visual field (can hold up fingers and have the patient tell you how many, or can have the patient tell you when your fingers start wiggling). Repeat the test with the other eye.
Pupillary reaction to light: follow the order of events below and you will get the most out of this exam:
- Shine penlight into one eye and observe the same eye for constriction.
- Shine penlight into the same eye again, and observe opposite eye for constriction.
- Repeat steps 1-2 for the other eye.
- Conduct swinging flashlight test, second eye should constrict slightly after flashlight moves to the other eye (direct stimulation of light is stronger than contralateral constriction compensation). Eye should most definitely NOT dilate
- Repeat step 5 for the other eye.
CN III, IV, & VI (OCCULAR MOVEMENTS)
Have the patient focus on either your finger or a pen, and move it in a “H” pattern (see below). Take note of any issues with ocular movement.
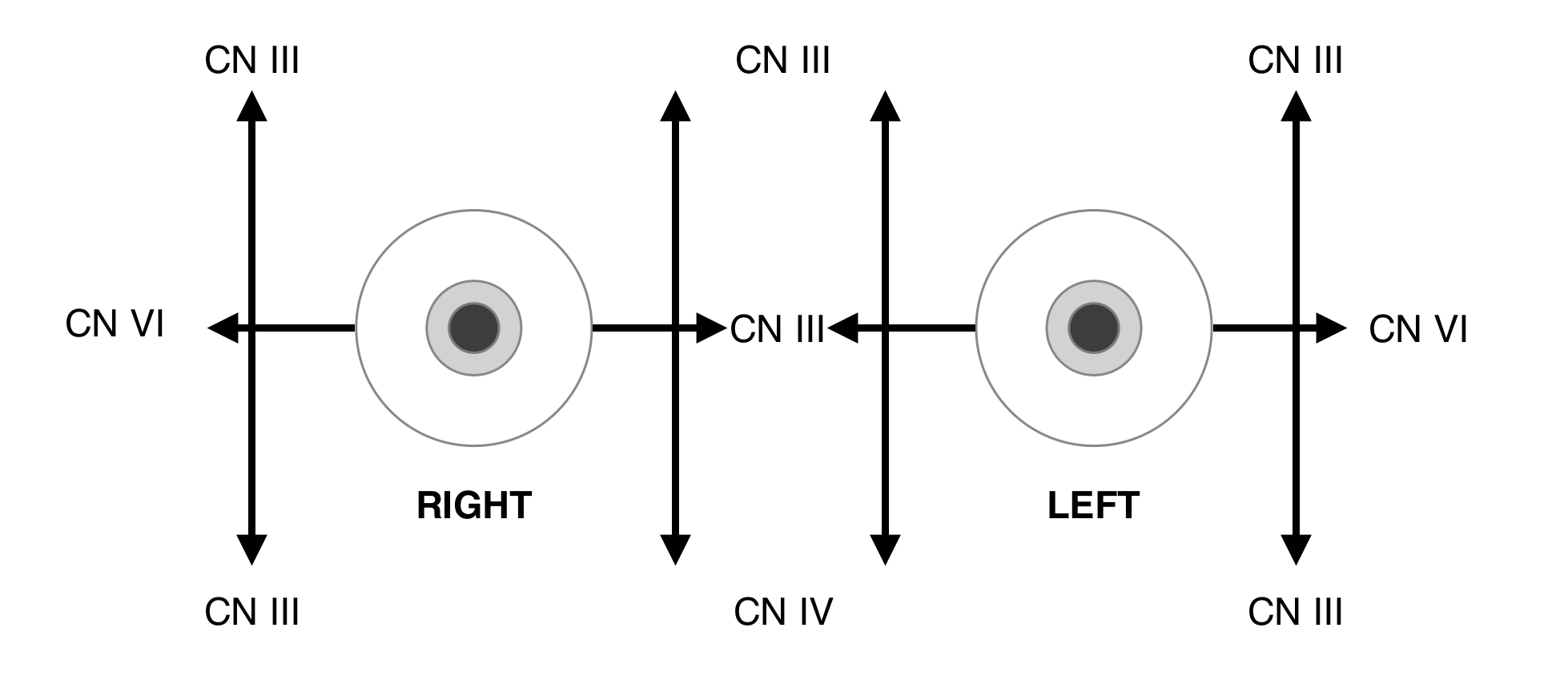
**CN III innervates every muscle except for the Superior Oblique (CN IV) and the Lateral Rectus (CN VI)
CN V (FACIAL SENSATION AND MASSETER EXAM)
Facial sensation: it is important to asses all 6 sectors (bilateral ophthalmic, maxillary and mandibular regions) for both types of sensation!
– Use a broken cotton swab to test for pinprick in all 6 areas (assess symmetry between right and left sides)
– Can use cool tuning fork to do the same (if time permits, however pinprick has already tested this sensory pathway)
– Use cotton swab end to assess fine touch (see if patient can tell which direction you move swab in each of the 6 regions)
Masseter exam: have patient clench teeth and feel for muscle contraction in the face. Can also feel for clenching in temporal muscles.
– Can also have patient open mouth and try to keep it open as you attempt to close jaw from below.
CN VII (FACIAL SYMMETRY/STRENGTH)
Other than normal observations (no ptosis, face droop, etc) you should assess upper and lower portions of the face (given separate innervation). Ideally have the patient conduct the following 3 things to look for weakness/asymmetry (WHILE noting where).
– Have the patient raise eyebrows
– Have patient shut eyes very tightly
– Have patient show all of their teeth/smile

CN VIII (HEARING)
There are 3 major parts to this portion of the exam.
1.) Rubbing finger test: can the patient hear you rubbing thumb/fingers next to each ear?
-Some like to whisper a number in one ear while rubing fingers in the other to see if patient can hear the number when distracted.
2.) Rinne test: strike 512 Hz tuning fork and hold base at mastoid bone. Follow these instructions below very carefully for both ears
– Ask patient if they can hear the fork when it is contact with the mastoid bone (they should be able to)
– Have the patient tell you the moment they no longer can hear the fork vibrating.
– As soon as this occurs hold the tines of the still vibrating fork next to the ear of the patient and ask if they can now again hear it. In a normal individual they should! The sound in the air medium should be louder than in the bone.
–If they can’t initially hear the fork, there is a sensory issue.
-If they can hear the fork initially, but it is not louder in the air medium, there is a conduction issue.
3.) Weber test: strike the 512 fork and hold base at the forehead. Ask patient where the sound is localizing. If the sound of the fork vibrating is equal in both ears, this is a normal result. If it localizes to one ear, their are two possibilities:
– The ear hearing more sound is abnormal and has a conduction issue (plugging a normal ear with a finger will replicate this phenomenon)
– The ear hearing less sound is abnormal and has a sensory issue.
CN IX, X (PALATE SYMMETRY AND ELEVATION):
Have the patient open their mouth and look back into the back of their throat. Have the patient swallow with their mouth open.
– Make sure the palate is able to be raised properly
– Check to make sure the uvula is and remains in the middle. The uvula will deviate away from the side of palate weakness (towards the strong/normal side)

CN XII (TONGUE SYMMETRY AND STRENGTH)
Have the patient stick out their tongue, and then move it side to side. The tongue will deviate toward the side of weakness/nerve damage.
– Can also check strength if desired (and if there is time): have patient push out their cheek from the inside of their mouth and oppose their movements.

CN XI (NECK TURN/SHOULDER SHRUG):
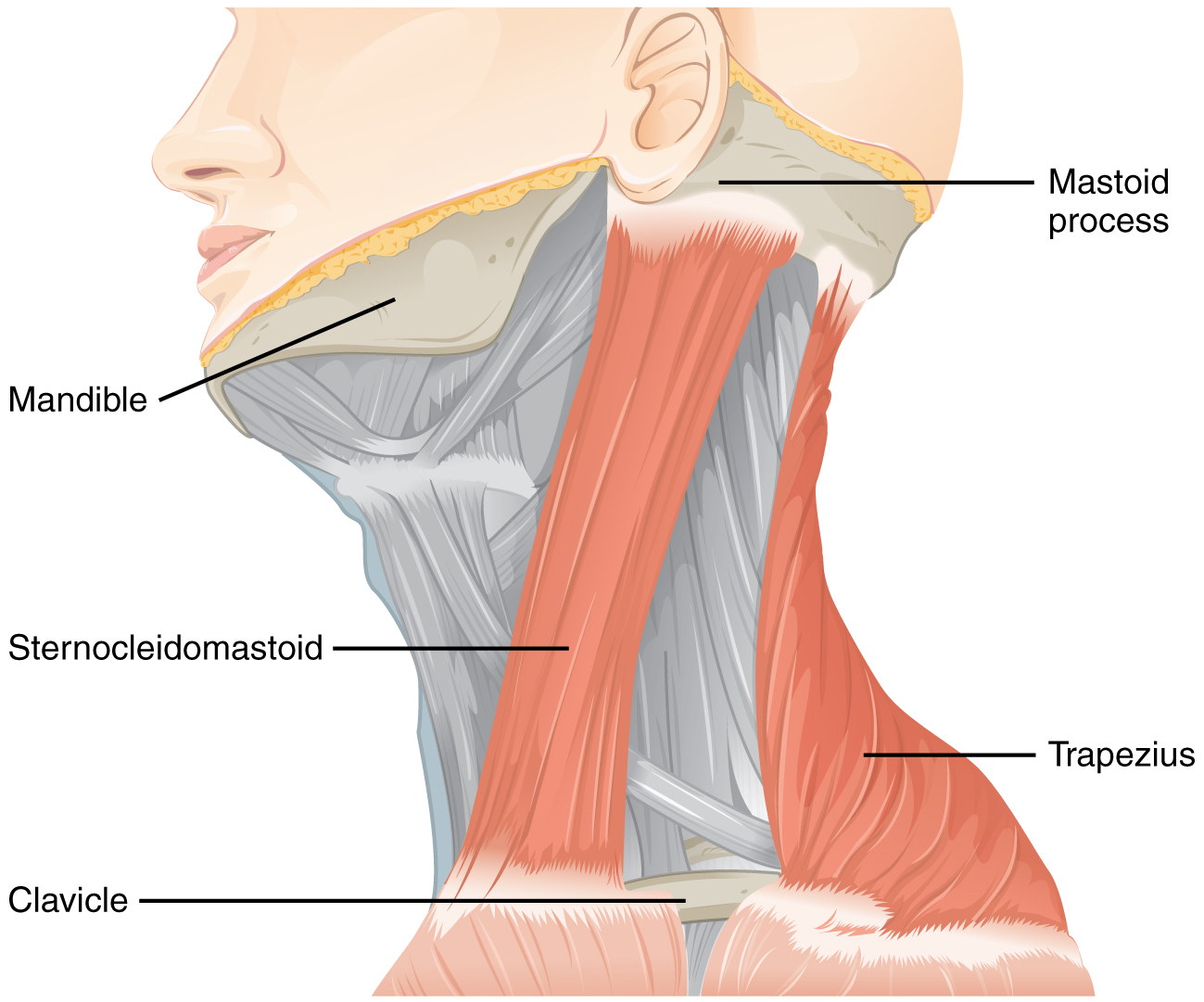
– Have the neck turn to each side. Turning to one direction tests the function of the sternocleidomastoid muscle on the opposite side. Oppose this turning movement to check strength.
-Have the patient shrug their shoulders (both together and one at a time). This movement can also be opposed to check for strength.
Page Updated: 01.20.2016