WHEN DO WE DO IT?
A cardiovascular exam (even if abridged) is typically done for most patients. With this in mind, many different chief complaints (i.e. shortness of breath, chest pain) can very well support the need to perform a more complete cardiovascular exam.
COMPONENTS
A complete cardiac exam has a few key components that we will discuss in more detail below.
- Inspection
- Palpation
- Auscultation
INSPECTION
Chest: Begin by inspecting the chest for any abnormalities, scars, signs of trauma, or dermatological findings (really anything of interest). Make sure to ask your patient about any unusual findings (every scar has a story!)
Edema: After examining the chest, take a quick look for peripheral edema that could be a sign of right heart failure (feel free to ask the patient questions about swollen ankles etc). If any edema is found apply pressure with your finger, and see if the edema filled tissue retains the imprint of your touch (i.e. pitting).

Nails: if not already inspected, look at the nails of the patient for any abnormal findings. Certain findings in the nail can be suggestive for specific conditions (such as splinter hemorrhages and infective endocarditis).

Jugular venous pulse (JVP): the information you find on this website for the analysis of the JVP will be different than what you might have read elsewhere. Realistically the JVP is an exam component that is not consistent and rarely accurate. That being said, the modified JVP visual exam discussed here can be useful. To begin with, the JVP simply refers to being able to witness the pressure wave (that is transmitted back form the right side of the heart) in the jugular vein. Why is this important? Because if you can see the JVP high up on the patients jugular vein they are likely volume overloaded (their vein is filled with a column of blood up until the point in which you can observe the pulsation).
The difficulty with this exam is that the JVP is not always clear to see (and the carotid pulse can sometimes masquerade as the JVP). First and foremost, look for the JVP in the path of the internal jugular vein shown below while the patient is sitting straight up:
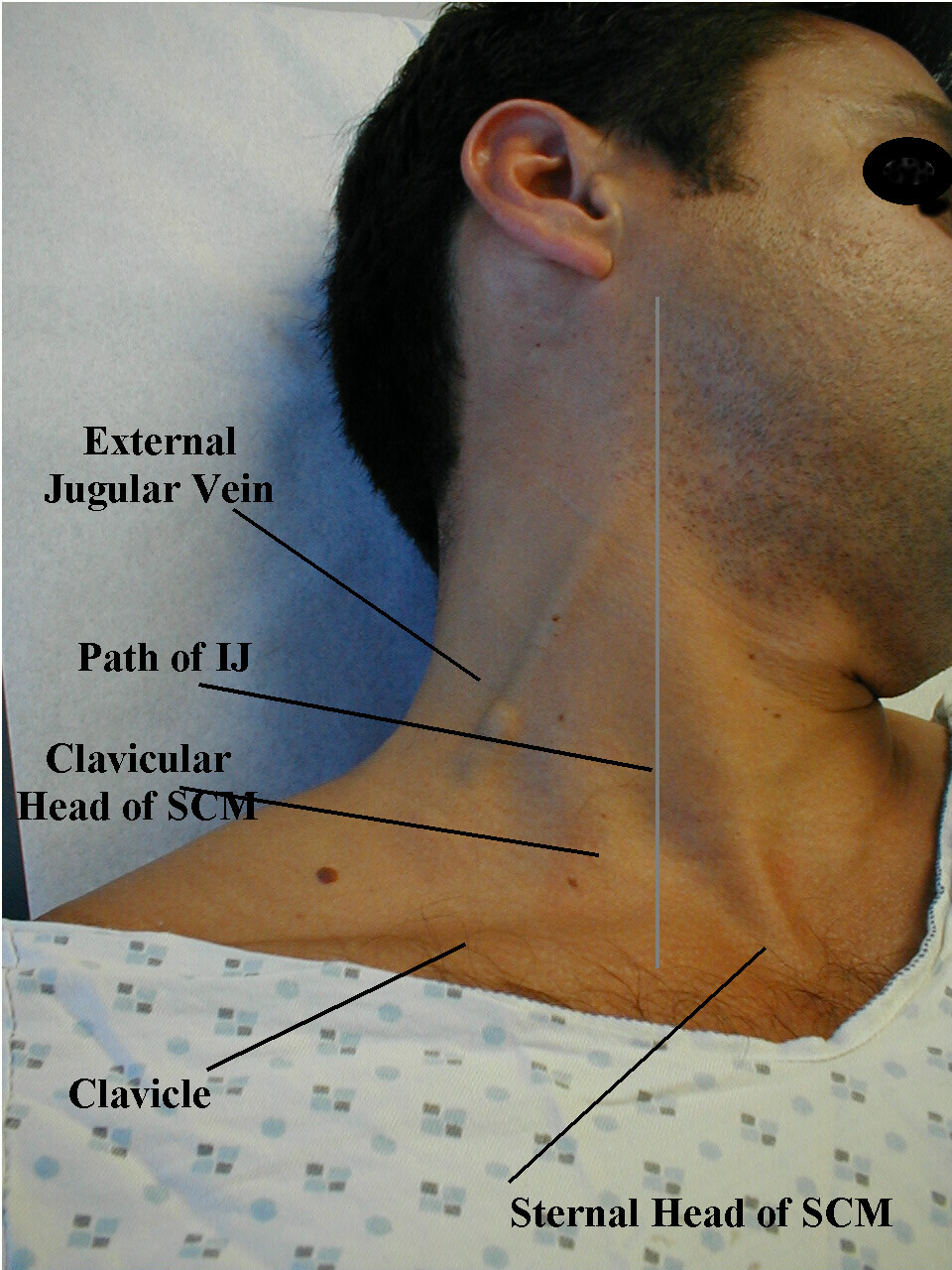
If any pulsation is present feel free to apply pressure to the neck in between the pulsation and the path leading to the heart. You should be able to compress the internal jugular vein (causing the pulsation to cease if it is in fact the JVP), and the carotid artery will not be compressive (the pressure is so high in this artery, that if your pulsation is caused by it, your application of pressure will not make the pulsation disappear). If the pulsation is present in the patient sitting upright, realistically this already is suggestive of volume overload (no further assessment is needed).
If no pulse is observable there are 3 major reasons for this
- This patient is difficult to appreciate a JVP on (i.e. your skills in the exam may need to be sharpened)
- The patient is very volume overloaded, to the point the JVP is above the area of observation (i.e. in the skull). If this is the case the patient will VERY likely have peripheral edema.
- The patient has an adequate volume or is volume depleted. Apply pressure to the liver while looking for a JVP (this will increase the column of blood in the jugular vein, allowing you to see the JVP in an individual who is neither volume overloaded or depleted. If you still can not observe a JVP, then it is suggestive that the patient might be volume depleted (check mucous membranes to see if they are moist, they will be dry if volume depleted).
PALPATION
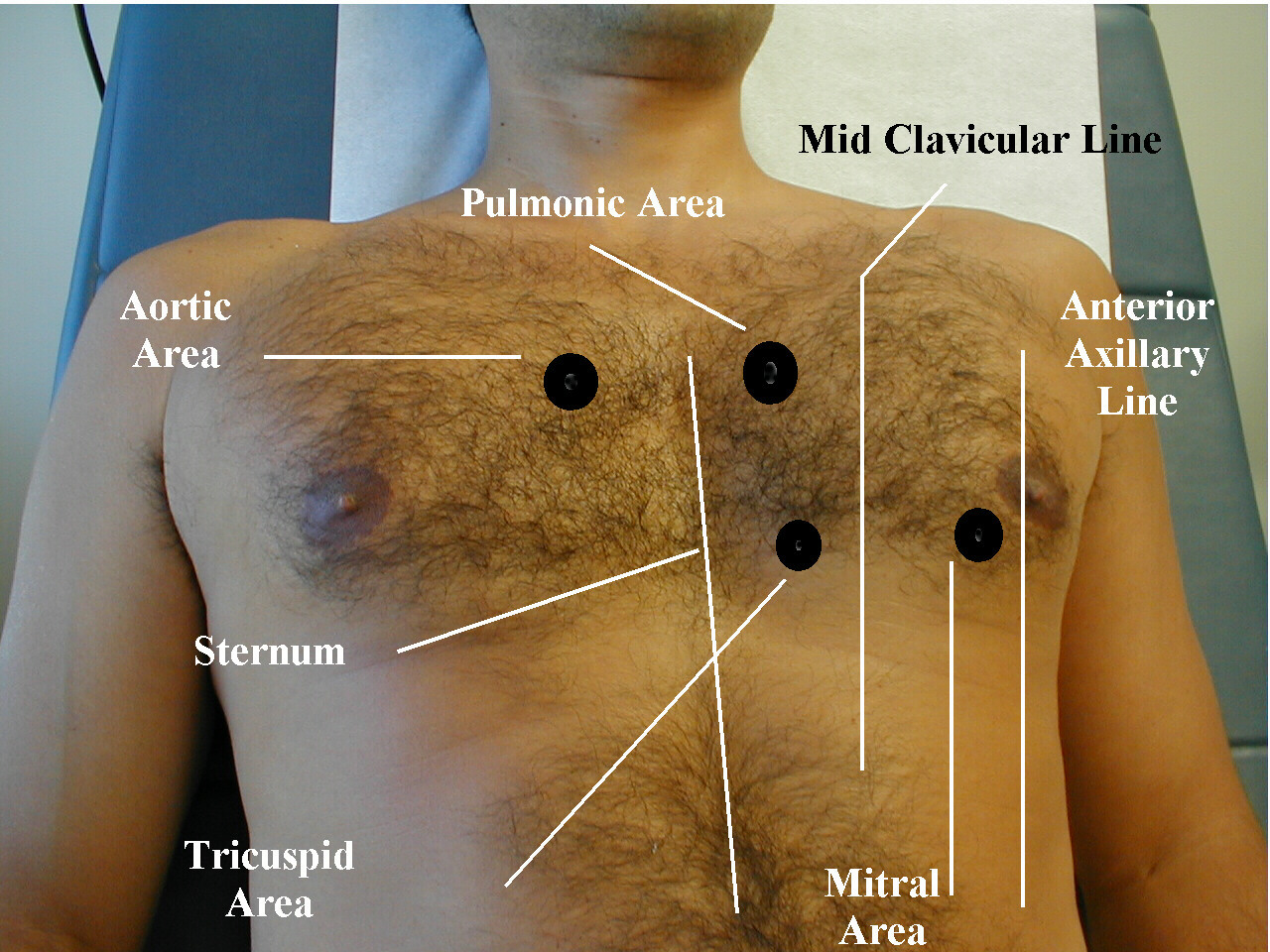
Point of maximal impulse: through the chest wall we are often able to feel the heart beat in a focused region called the point of maximal impulse. Generally speaking this should be around the mid clavicular line and the size of a quarter. Deviation can suggest an altered cardiac axis, or even underlying cardiac pathologies. Feel for the point of the maximal impulse in the manner shown below using the palm of your hand.

*Feel over the regions of the heart for the presence of any thrills (murmurs whose vibrations can be sensed)
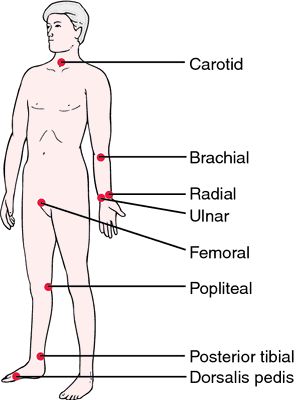
Pulses: there are various different places on the patient where you can try and feel for a pulse. These include: carotid, brachial, radial, ulnar, femoral, popliteal, dorsalis pedis, posterior tibial. The specific pulse you chose to take might depend on the clinical context you are in.
AUSCULTATION
Heart sounds: using your stethoscope listen for normal S1 and S2 heart sounds (as well as extra heart sounds such as S3 or S4) at the aortic, pulmonic, tricuspid, and mitral valve locations.
- An S3 heart sound is associated with heart failure (among other things) and is thought to be the sound of rapid ventricular filling
- An S4 year sound caused during atrial contraction, and is believed to be the sound of blood hitting a hardened/stiffened ventricle (suggestive of hypertrophy of the heart).
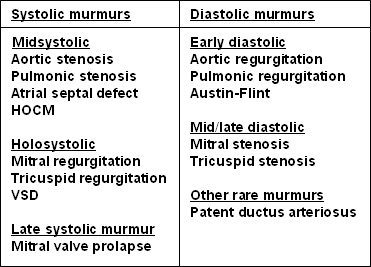
Murmurs: while listening at the above locations, make sure to keep an ear out for any usual murmurs. Some examples of conditions that cause characteristic murmurs are below.
Page Updated: 01.19.2016