Page Contents
WHAT IS IT?
Chronic lymphocytic leukemia (CLL) refers to a hematologic cancer that is characterized by progressive accumulation of mature malignant B-cell lymphocytes in peripheral blood and bone marrow. Given its name, it is a slow progressing disease unlike acute lymphoblastic leukemia.
Technically speaking, the involvement of lymph nodes leads to a diagnosis called small lymphocytic lymphoma (SLL). It is important to realize for classification purposes that in CLL most of the malignant cells are in the circulation/bone marrow, while in SLL they are mostly localized if focal masses (often in lymph nodes, but can also be outside the node).
Cause: a variety of survival signaling pathways (involving the B-cell, chemokine, and cytokine receptors) are implicated in the genesis of this disease.
WHY IS IT A PROBLEM?
Bone marrow infiltration of malignant cells can disrupt erythropoiesis/platelet formation and lead to anemia/thrombocytopenia (normal hematopoietic cells become overwhelmed). Furthermore it is believed that CLL can even be responsible for mediating an autoimmune mechanism of red blood cell destruction (autoimmune hemolytic anemia).
Patients are also predisposed to infection, as many of them develop low levels of antibodies (hypogammaglobulinemia) within the blood due to mysterious mechanisms mediated by CLL. The most common cause of death in patients with CLL is infection.
WHAT MAKES US SUSPECT IT?
Risk factors: old age (>60), male
*Majority of patients are asymptomatic
Chief complaints: for the minority who do have symptoms, these are the common complaints patients experience (also called B symptoms)
- Night sweats
- Weight loss
- Weakness/fatigue (likely due to the anemia)
- Fever (medically unexplained).
Physical exam findings: swollen lymph nodes (most common), enlarged spleen, and/or enlarged liver.
HOW DO WE CONFIRM A DIAGNOSIS?
Complete blood count (CBC): these are the likely findings in a patient with CLL:
- Increased white blood cell count (WBC) with increased lymphocytes specifically *the higher this white count, the worse the prognosis
- Low hemoglobin (can be normocytic, but also macrocytic if folate is also low)
- Low platelets (thrombocytopenia)
Blood smear: can visualize “smudge cells” (also called “smear cells”) on peripheral blood smear. These are fragile lymphocytes (which are clonal B-cells produced in CLL) that are small, round , and have small cytoplasms. They are physically crushed during the process of preparing the blood smear slide (resulting in their characteristic appearance).
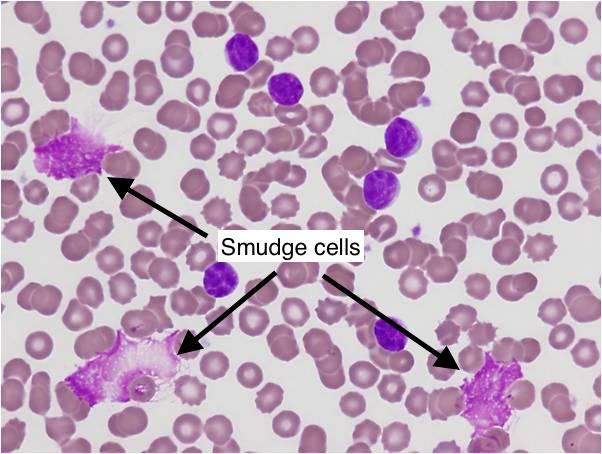
The total number of lymphocytes will be increased as well on the smear, however there will be little or no blast cells.
Bone marrow biopsy will demonstrate less than 10% blast cells (although biopsy is not required for diagnosis)
Immunohistochemmistry (IHC): Tumor cells (in the bone marrow, blood, and/or lymph nodes) will express cell markers CD19, CD20, and also CD5 (the last of which is only present on normal T-cells). Presence of CD5 on a B cell identifies it as malignant.
Flow cytometry can be used to confirm the clonality of the B-cells present in the patients blood.
*Some patients might have a monoclonal Ig spike given that this is the clonal expansion of a B-cell lineage
Lymph node biopsy (for SLL): can diagnose invasion of a lymph node with malignant B cells.
HOW DO WE TREAT IT?
The disease is slow progressing, so care is geared towards control symptoms vs. curing it. Many are not treated until they develop symptoms that affect their quality of life (such as the B symptoms stated above).
Typical treatments:
Chemoimmunotherapy: this refers to a combination of chemotherapy (using a medication such as Cyclophosphamide, that adds an Alkyl group to DNA, inducing death in cells) with immune modulatory medications. Some options of immune therapies include:
- Alemtuzumab: this is a therapeutic antibody that targets CD52 (surface marker on mature lymphocytes).
- Rituximab: Monoclonal antibody that targets CD20 (found on B-cells). Facilitates destruction of B-cells.
- Prednisone: Glucocorticoids that is commonly used in CLL chemotherapy.
Purine analogs: these medications that mimic purines (that are incorporated into DNA) are also used to manage CLL. One example that is commonly used is Fludarabine that is a guanosine analog that is capable of inhibiting DNA replication enzymes (DNA polymerases, DNA primase, and DNA ligase). These analogs can be used in combination with chemoimmunotherapy.
*Treating CLL is complicated and needs to be tailored to the specific biology of the patient, the above information is only the tip of the iceberg with regards to treatment options for patients (as well as the approach needed to analyze the specific biology that underlies a particular patient with CLL.
HOW WELL DO THE PATIENTS DO?
Average survival is about ~5 years, however some might survive for longer than 10 years if initial cancer burden is modest.
WAS THERE A WAY TO PREVENT IT?
While the cancer itself can not be prevented, infections that ultimately cause death can. Antiviral therapy can be used as prophylaxis, and patients should avoid any type of live vaccination when immunocompromised.
WHAT ELSE ARE WE WORRIED ABOUT?
Autoimmune hemolytic anemia (warm and cold) can be seen in patients with CLL.
Richter transformation; this is transformation of the cancer to a diffuse large B-cell lymphoma. Can be marked clinically by an enlarged lymph node or spleen.
OTHER HY FACTS?
Chromosomal translocations are rare in CLL/SLL (unlike other lymphoid malignancies)
This is the most common adult leukemia.
B-cells that are neoplastic are CD20 and CD5 positive.
Page Updated: 01.11.2016